Angiotensin
Template:BsdRobert Tito | Talk 18:40, 20 February 2007 (CST)
Angiotensinogen
| |
| Identifiers | |
| Symbol(s) | AGT |
| Entrez | 183 |
| OMIM | 106150 |
| RefSeq | NM_000029 |
| UniProt | P01019 |
| Other data | |
| Locus | Chr. 1 q41-qter |
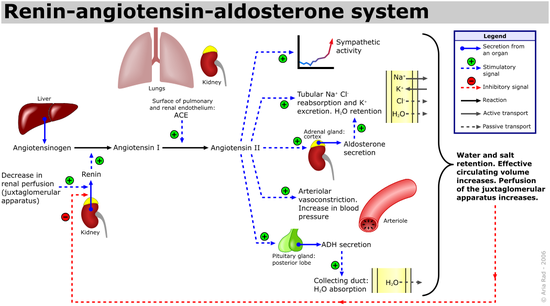
Angiotensin is an oligopeptide hormone that circulates in the blood and which causes vasoconstriction, increased blood pressure, and release of aldosterone from the adrenal cortex. It is also a powerful dipsogen as a result of its actions on the brain. It is derived from the precursor molecule angiotensinogen, a serum globulin produced in the liver. It plays an important role in the renin-angiotensin system, an endocrine system that helps regulate long-term blood pressure and blood volume in the body. The system can be activated when there is a loss of blood volume or a fall in blood pressure (such as in a hemorrhage).
- If the perfusion of the juxtaglomerular apparatus in the kidneys decreases, then the juxtaglomerular cells release the enzyme renin.
- Renin cleaves an inactive peptide called angiotensinogen, converting it into angiotensin I.
- Angiotensin I is then converted to angiotensin II by angiotensin-converting enzyme (ACE), which is found mainly in lung capillaries.
Angiotensinogen is an α-2-globulin that is produced constitutively and released into the circulation mainly by the liver, although other sites are thought to be involved also. It is a member of the serpin family, although it is not known to inhibit other enzymes, unlike most serpins. Plasma concentrations of angiotensinogen are increased by plasma corticosteroid, estrogen, thyroid hormone, and angiotensin II levels. Angiotensinogen has 453 amino acid residues.
Angiotensin I (Asp-Arg-Val-Tyr-Ile-His-Pro-Phe-His-Leu) (CAS# 11128-99-7) is formed by the action of renin on angiotensinogen. Renin is produced in the kidneys in response to both decreased intra-renal blood pressure at the juxtaglomerular cells, or decreased delivery of Na+ and Cl- to the macula densa. If more Na+ is sensed, renin release is decreased. Renin cleaves the peptide bond between the leucine (Leu) and valine (Val) residues on angiotensinogen, creating the decapeptide (des-Asp) angiotensin I (CAS# 9041-90-1). Angiotensin I appears to have no biological activity and exists solely as a precursor to Angiotensin II (Asp-Arg-Val-Tyr-Ile-His-Pro-Phe | His-Leu)
Angiotensin I is converted to angiotensin II through removal of two terminal residues by the enzyme Angiotensin-converting enzyme (ACE, or kininase), which is found predominantly in the capillaries of the lung. ACE is a target for inactivation by ACE inhibitor drugs, which reduce the rate of angiotensin II production. Other cleavage products, 7 or 9 amino acids long, are also known; they have differential affinity for angiotensin receptors, although their exact role is still unclear. The action of angiotensin II itself is targeted by angiotensin II receptor antagonists, which directly block angiotensin II AT1 receptors. Angiotensin II is degraded to angiotensin III by angiotensinases that are located in red blood cells and the vascular beds of most tissues. It has a half-life in the systemic circulation of about 30 seconds, but in tissue, it may be as long as 15-30 minutes.
'Angiotensin III (Asp | Arg-Val-Tyr-Ile-His-Pro-Phe) has 40% of the pressor activity of angiotensin II, but 100% of the aldosterone-producing activity.
Angiotensin IV (Arg | Val-Tyr-Ile-His-Pro-Phe) is a hexapeptide which, like angiotensin III, has some lesser activity.
Effects of angiotensins
Angiotensin I has relatively little activity, but angiotensin II has a variety of physiologically important actions:
- Throughout the body, angiotensin II is a potent direct vasoconstrictor, constricting arteries and veins and increasing blood pressure. It also has prothrombotic potential through adhesion and aggregation of platelets and production of PAI-1 and PAI-2. It has been proposed that angiotensin II could be a cause of vascular and cardiac muscle hypertrophy (enlargement of the heart).
- In the kidneys, it constricts glomerular arterioles, having a greater effect on efferent arterioles than on afferent arterioles. As with most other capillary beds in the body, the constriction of afferent arterioles increases the arterioler resistance, raising systemic arterial blood pressure and decreasing the blood flow. However, the kidneys must continue to filter enough blood despite this drop in blood flow, necessitating mechanisms to keep glomerular blood pressure up. To do this, Angiotensin II constricts efferent arterioles, which forces blood to buildup in the glomerulus, increasing glomerular pressure. The glomerular filtration rate (GFR) is thus maintained, and blood filtration can continue despite lowered overall kidney blood flow. Angiotensin II has a direct effect on the proximal tubules to increase resorption of sodium. Although it slightly inhibits glomerular filtration by indirectly (through sympathetic effects) and directly stimulating mesangial cell constriction, its overall effect is to increase the glomerular filtration rate by increasing the renal perfusion pressure via efferent renal constriction.
- Angiotensin II increases thirst(i.e.it is a potent dipsogen) through its actions on the subfornical organ, one of the circumventricular organs of the brain; it also decreases the response of the baroreceptor reflex, and it increases the salt appetite¦desire for salt. It increases the secretion of vasopressin from the posterior pituitary and of ACTH from the anterior pituitary. It also potentiates the release of norepinephrine by direct action on postganglionic sympathetic fibers.
- Angiotensin II acts on the adrenal cortex to cause the release of the mineralocorticoid hormone aldosterone. Aldosterone acts on the tubules (i.e. the distal convoluted tubules and the cortical collecting ducts) in the kidneys, causing them to reabsorb more sodium and water from the urine. Potassium is secreted into the tubule in exchange for the sodium, which is reabsorbed. Aldosterone also acts on the central nervous system to increase a person's appetite for salt, and to make them feel thirsty.Elevated plasma angiotensin II levels are responsible for the elevated aldosterone levels during the luteal phase of the menstrual cycle.
These effects directly act to increase the amount of fluid in the blood, making up for a loss in volume, and to increase blood pressure.
Clinical significance
The renin-angiotensin system is often manipulated clinically to treat high blood pressure. Inhibitors of angiotensin-converting enzyme (ACE inhibitors) are often used to reduce the formation of the more potent angiotensin II. Alternatively, angiotensin receptor blockers can be used to prevent angiotensin II from acting on angiotensin receptors.
Interestingly, ACE cleaves a number of other peptides, and in this capacity is an important regulator of the kinin-kallikrein system.
Angiotensin Receptors
angiotensin II receptor, type 1
| |
| Identifiers | |
| Symbol(s) | AGTR1 AGTR1B |
| Entrez | 185 |
| OMIM | 106165 |
| RefSeq | NM_000685 |
| UniProt | P30556 |
| Other data | |
| Locus | Chr. 3 q21-q25 |
angiotensin II receptor, type 2
| |
| Identifiers | |
| Symbol(s) | AGTR2 |
| Entrez | 186 |
| OMIM | 300034 |
| RefSeq | NM_000686 |
| UniProt | P50052 |
| Other data | |
| Locus | Chr. X q22-q23 |
The angiotensin receptors are G protein-coupled receptors responsible for the signal transduction of the main effector hormone. The AT1 and AT2 receptors have a sequence identity of ~30%, but have a similar affinity for angiotensin II, their main ligand.
The AT1 receptor is the best elucidated angiotensin receptor. It is coupled to phospholipase C and angiotensin II increases the cytosolic Ca2+ level. It also inhibits adenylate cyclase and activate various tyrosine kinases. Effects mediated by the AT1 receptor include vasoconstriction, aldosterone synthesis and secretion, increased vasopressin secretion, cardiac hypertrophy, augmentation of peripheral noradrenergic activity, vascular smooth muscle cells proliferation, decreased renal blood flow, renal renin inhibition, renal tubular sodium reuptake, modulation of central sympathetic nervous system activity, cardiac contractility, central osmocontrol and extracellular matrix formation.
AT2 receptors are more plentiful in the foetus and neonate. Effects mediated by the AT2 receptor include inhibition of cell growth, fetal tissue development, modulation of extracellular matrix, neuronal regeneration, apoptosis, cellular differentiation and maybe vasodilation. Other poorly characterized subtypes include AT3 receptor and AT4 receptor. The AT4 receptor is activated by angiotensin IV, and may play a role in regulating the CNS extracellular matrix.
- IUPHAR GPCR Database - Angiotensin Receptors
- Online Mendelian Inheritance in Man, OMIM®. Johns Hopkins University, Baltimore, MD. MIM Number: 106165. World Wide Web URL: http://omim.org/. (AGTR1), Online Mendelian Inheritance in Man, OMIM®. Johns Hopkins University, Baltimore, MD. MIM Number: 300034. World Wide Web URL: http://omim.org/. (AGTR2)