Stroke: Difference between revisions
imported>Peter A. Lipson |
mNo edit summary |
||
| (120 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
{{subpages}} | |||
{{TOC|right}} | |||
A '''stroke''' (''syn. Cerebral Vascular Accident or "CVA"'') is a sudden, often focal, loss of [[brain]] function. "Cerebral vascular accident" summarizes features of a stroke: (1) "cerebral" (brain) (2) "vascular" (blood supply) and (3) "accident" indicates that this is a rapid and detrimental event. Although most strokes in people ''do'' involve the higher centers of the brain that are located in the [[cerebral hemisphere]]s; the word cerebral is not strictly accurate, as some strokes can involve ''only'' the lower portions of the brain, like the [[medulla oblongata]] or other areas of the [[brain stem]]. Most stroke experts prefer the term "stroke" to "CVA", but both are used commonly to refer to this acquired neurological disorder. The term "'''brain attack'''" has been advocated for use in the United States for stroke, just as the term "heart attack" is used for [[myocardial infarction]], to reinforce the idea that urgent treatment of developing stroke is essential. | |||
Many hospitals have multidisciplinary "stroke teams" specifically for swift treatment of stroke. While an [[emergency medicine|emergency physician]] may first see the patient, [[neurology|neurologists]], [[neurosurgery|neurosurgeons]] and [[radiology|interventional radiologists]] may quickly become involved. The patient is apt to need both immediate [[critical care]] and long term rehabilitation. | |||
For survivors of stroke, treatment is important in three distinct phases after the incident. Immediate treatment in the minutes and hours after the first signs of a stroke can sometimes change the course of the acute event by removing factors (like an embolus or extreme hypertension) that will otherwise promote greater and greater injury. Treatment ''after'' the acute stroke [[physical and rehabilitation medicine|rehabilitation therapy]] can offer the best hope of maximal recovery for most patients by aiding the person's ability to use their surviving brain to take over some of the functions that damaged tissues cannot manage, and long term therapy can help reduce the underlying risks of another stroke. | |||
==Epidemiology== | ==Epidemiology== | ||
Stroke is one of the leading causes of long term | Stroke is one of the leading causes of long term disability, and of death, in the developed world. Approximately 700,000 Americans per year experience a stroke. It is the third leading cause of death and the leading cause of long-term adult disability in the United States.<ref>Centers for Disease Control and Prevention (CDC). Prevalence of disabilities and associated health conditions among adults: United States, 1999. MMWR Morb Mortal Wkly Rep. 2001; 50: 120–125</ref> On average, a stroke occurs every 45 seconds and someone dies from a stroke every 3 minutes.<ref>Circulation. 2007;115:e69-e171.</ref><ref>http://circ.ahajournals.org/cgi/content/full/CIRCULATIONAHA.106.179918</ref> | ||
It is the third leading cause of death and the leading cause of long-term adult disability in the United States.<ref>Centers for Disease Control and Prevention (CDC). Prevalence of disabilities and associated health conditions among adults: United States, 1999. MMWR Morb Mortal Wkly Rep. 2001; 50: 120–125</ref> On average, a stroke occurs every 45 seconds and someone dies from a stroke every 3 minutes.<ref>Circulation. 2007;115:e69-e171.</ref><ref>http://circ.ahajournals.org/cgi/content/full/CIRCULATIONAHA.106.179918</ref> | |||
Asymptomatic infarctions, usually lacunar, are present in 7% of MRI scans; 2% of scans detect incidental [[intracranial aneurysm]]s.<ref name="pmidpending-nejm">Vernooij MW et al. Incidental Findings on Brain MRI in the General Population. New Eng J Med 2007. http://content.nejm.org/cgi/content/abstract/357/18/1821</ref> | |||
Risk factors for stroke include [[atherosclerosis]], advanced age, [[hypertension]] (high blood pressure), [[diabetes mellitus]], [[hypercholesterolemia|high cholesterol]], [[cigarette smoking]], [[atrial fibrillation]], [[migraine headache]]s<ref name="pmid19861375">{{cite journal| author=Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T| title=Migraine and cardiovascular disease: systematic review and meta-analysis. | journal=BMJ | year= 2009 | volume= 339 | issue= | pages= b3914 | pmid=19861375 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=19861375 | doi=10.1136/bmj.b3914 }} <!--Formatted by http://sumsearch.uthscsa.edu/cite/--></ref>, ethnic identity, and some blood clotting disorders. | |||
==Causes== | |||
There are many different causes of stroke, but whenever a stroke occurs, there has been an interruption of the normal blood supply to brain cells that has gone on long enough to cause death to at least some of them. If the loss is so brief that the brain tissue can quickly recover, and does not die, then a [[Transient Ischemic Attack (TIA)]] has occurred, rather than a stroke.The symptoms and signs of a stroke are highly dependent upon the number of cells that are affected, and exactly where these cells are located in the brain. Accordingly, strokes can have ''many'' different clinical presentations - ranging from deep coma with the loss of the ability to breathe; to ''very'' limited deficits in the ability to move a part of the body, or changes in sensory perception like partial blindness from a restriction in visual field, without any associated problems with movement. | |||
The interruption of blood circulation generally comes about either because (1) blood flow is stopped (occluded) within the blood vessel, or because (2) the blood vessel ruptures (hemorrhages). In either case, the vessel no longer serves to supply the brain cells with nutrients and oxygen. Hemorrhages hurt the brain in ways besides starving cells, the break in the vessels from a hemmorrhage floods the blood it carries into an expanding clot that also causes damage from excessive pressure. | |||
Ordinarily, at least ''some'' brain tissue is injured by a stroke - yet not killed. The injury to these cells is reversible. That's one reason why the amount of recovery during the initial time period after a stroke is difficult to predict, and also why treatment at that time can influence the course of recovery. If the stroke patient survives the stroke, some brain cells may actually recover in time if the injury was not too great. Since the [[central nervous system]], even in older adults, has at least some ability to adjust to loss of ([[plasticity]]), such that other areas of the brain can often take over partial functions of the damaged areas, there may be more recovery of function over time for the patient, even once the damaged areas of the brain are no longer capable of any additional recovery of injured brain cells. | |||
== | ==Anatomy== | ||
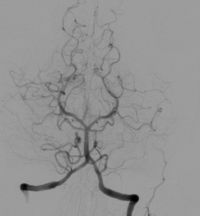
[[Image:Cerebral angiography, arteria vertebralis sinister injection.JPG|200px|thumb|right|Angiographic image of normal cerebral anatomy| This illustration serves to show the reader the ''general'' circular shape of the roadmap of arteries that supply the brain. This is an x-ray image of the head after a radio-opaque dye was injected into the arterial system, the image is called an [[Angiogram|angiogram]]. For more detailed discussion of anatomy, see [[Circle of Willis]]. ]] | |||
The brain is made out of nerve cells and supporting cells, it is covered by protective layers and it is moistened by the constant circulation of a pristine fluid called "[[cerebrospinal fluid]]" (CSF). | |||
Like all parts of the body, the brain has vessels that pump blood to it from the [[Heart|heart]] called [[Artery|arteries]] and vessels that collect the blood after circulating through the organ for return to the heart called [[Vein|veins]]. As in most organs of the body, the arteries to the brain carry blood loaded with oxygen and glucose (blood sugar) and the veins carry away blood that has delivered these vital supplies to the cells of the brain and had their waste products dumped in it. | |||
There are ''special'' features of the vasculature to the brain that are protective since brain cells are ''more vulnerable'' to loss of oxygen and glucose than are the cells of any other portion of the body. One of these features is the ''circular'' design of the blood delivery system to the brain. This ''circle'' of arteries that joins blood pumped up from the front of the [[Neck|neck]] ( the carotid arteries) from blood pumped up from the back (the vertebral arteries). In most healthy young people, this system of blood flow is so good that even if one of the arteries is lost altogether (from an injury, for example), the others can make up for it and keep delivering a properly working circulation of fresh arterial blood, and no impairment to the brain cells occurs. | |||
== | ==Classification of Strokes== | ||
''' | '''This section aims to lay out the types of strokes so that the rest of the article is more easily understood. Strokes can be classified according to the mechanism of injury, and also according to the areas of the brain that are injured. Need to reorganize to have "classification", then specific types/subtypes. | ||
''' | |||
Strokes can be classified as '''ischemic''' or '''hemorrhagic'''. In ischemic strokes, all or part of the brain is deprived of blood and oxygen, usually through the blockage of an artery. In hemorrhagic strokes, loss of blood supply plays a part, but the initial event is bleeding into the brain causing increased pressure on the brain, and irritation to brain tissue. | |||
====Embolic Stroke==== | ====Ischemic strokes==== | ||
The word [[ischemia]] indicates the loss of blood supply to tissues. When tissues are ischemic, they are generally pale and, if the ischemia persists long enough, become swollen and change further as cells swell and then die. The area of dead (also called necrotic) tissue that results from ischemia is called an [[Infarct|infarct]]. | |||
*Ischemic strokes make up about 87% of all strokes and can be due to blockage of a feeding artery by a clot or by generalized low blood flow (hypoperfusion), along with narrowed arteries. ''Lacunae'', or small vessel ischemic strokes, are responsible for about 20% of all strokes and are common in hypertension and [[diabetes mellitus]]. | |||
*[[Hemorrhagic stroke]]s are usually classed as either [[intracerebral hemorrhage]] or [[subarachnoid hemorrhage]].<ref>Goldman: Cecil Textbook of Medicine, 22nd ed., Copyright © 2004 W. B. Saunders Company</ref> Uncontrolled hypertension is a leading cause of hemorrhagic stroke. Weaknesses in brain arteries, (for example, [[intracranial aneurysm]]s) can cause hemorrhagic strokes even when the pressure of the blood inside the arteries is not excessive. Because the brain is enclosed within a rigid structure (the [[skull]]), even a small amount of bleeding can cause a dramatic increase in pressure on the brain. This can lead to ''herniation'', in which part of the brain is compressed through the base of the skull, causing rapid coma and death. | |||
'''[[Atherosclerosis]]''' is responsible for the majority of ischemic strokes. The etiology of atherosclerosis-related strokes is very similar to that of heart attacks. An [[atherosclerotic plaque]] in a cerebral artery can gradually develop an associated thrombus or rupture suddenly causing a rapid occlusion, or the thrombus can break off and lodge in a vessel even deeper in the brain. "Thrombotic stroke" usually refers to in-situ thrombus, "embolic stroke" to thrombi that travel from distant sites. | |||
=====Thrombotic Stroke===== | |||
Thrombotic and thromboembolic strokes can originate in either large or small blood vessels, and are usually due to abnormalities in the vessel (most commonly [[atherosclerosis]]). Atheroembolism can occur within the cerebral circulation or can originate outside the cerebral circulation. One of the most important etiologies is [[carotid artery disease]]. Lacunae are also a subset of thrombotic stroke. | |||
=====Embolic Stroke===== | |||
Embolism of thrombi from outside the cerebral circulation are responsible for a large and important subset of ischemic strokes. In these cases a thrombus (blood clot) travels from its origin and lodges in a cerebral artery. Most of these strokes are of cardiac origin (Cardioembolic). | Embolism of thrombi from outside the cerebral circulation are responsible for a large and important subset of ischemic strokes. In these cases a thrombus (blood clot) travels from its origin and lodges in a cerebral artery. Most of these strokes are of cardiac origin (Cardioembolic). | ||
| Line 42: | Line 54: | ||
*Mural thrombi: anything that causes blood flow in the heart to slow can cause thrombus formation. This includes thrombi formed in the atrial appendage and thrombi formed in the left ventricle in patients with heart failure. | *Mural thrombi: anything that causes blood flow in the heart to slow can cause thrombus formation. This includes thrombi formed in the atrial appendage and thrombi formed in the left ventricle in patients with heart failure. | ||
*Valvular heart disease: this includes [[rheumatic heart disease]], [[infective endocarditis]], and presence of a prosthetic heart valve. | *Valvular heart disease: this includes [[rheumatic heart disease]], [[infective endocarditis]], and presence of a prosthetic heart valve. | ||
*Paradoxical embolism: this occurs primarily when a | *Paradoxical embolism: this occurs primarily when a thrombosis elsewhere in the body breaks off, passing through a [[patent foramen ovale]] (PFO) into the left ventricle (especially if an atrial septal aneurysm is present), and then to the brain.<ref name="pmid18046029">{{cite journal |author=Handke M, Harloff A, Olschewski M, Hetzel A, Geibel A |title=Patent foramen ovale and cryptogenic stroke in older patients |journal=N. Engl. J. Med. |volume=357 |issue=22 |pages=2262–8 |year=2007 |pmid=18046029 |doi=10.1056/NEJMoa071422}}</ref> | ||
====Systemic hypoperfusion (Watershed stroke)==== | ====Systemic hypoperfusion (Watershed stroke)==== | ||
| Line 55: | Line 67: | ||
====Subarachnoid hemorrhage==== | ====Subarachnoid hemorrhage==== | ||
Subarachnoid hemorrhage (SAH) is bleeding into the [[cerebrospinal fluid]] (CSF) surrounding the brain. The two most common causes of SAH are rupture of [[ | Subarachnoid hemorrhage (SAH) is bleeding into the [[cerebrospinal fluid]] (CSF) surrounding the brain. The two most common causes of SAH are rupture of [[intracranial aneurysm]] and bleeding from [[vascular malformations]]. Bleeding into the CSF from a ruptured aneurysm occurs very quickly, causing rapidly increased [[intracranial pressure]]. The initial bleed can be brief, but rebleeding is common. Death or deep coma ensues if the bleeding continues. SAH has a 37-45% mortality for patients 45 and older.<ref>El-Saed A, Kuller LH, Newman AB, Lopez O, Costantino J, McTigue K, Cushman M, Kronmal R. Geographic variations in stroke incidence and mortality among older populations in four US communities. Stroke. 2006; 37: 1975–1979.</ref><ref>Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, Copper LS, Shahar E. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerotic Risk in Communities (ARIC) Cohort. Stroke. 1999; 30: 736–743</ref> [[Intracranial aneurysm]] can be associated with other disorders, such as [[adult polycystic kidney disease]]. | ||
==Risk Factors== | ==Risk Factors== | ||
| Line 84: | Line 96: | ||
==Diagnosis== | ==Diagnosis== | ||
A stroke is diagnosed first by a medical professional taking a proper history and physical exam. | A stroke is diagnosed first by a medical professional taking a proper history and physical exam. However, 13% of suspected strokes may actually be a [[seizure]], [[migraine]] headache, or conversion disorder.<ref name="pmid20335564">{{cite journal| author=Chernyshev OY, Martin-Schild S, Albright KC, Barreto A, Misra V, Acosta I et al.| title=Safety of tPA in stroke mimics and neuroimaging-negative cerebral ischemia. | journal=Neurology | year= 2010 | volume= 74 | issue= 17 | pages= 1340-5 | pmid=20335564 | ||
*Computed tomography (CT) scan | | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20335564 | doi=10.1212/WNL.0b013e3181dad5a6 }} </ref> Tests include: | ||
*Magnetic resonance imaging (MRI) | * [[Computed tomography]] (CT) scan | ||
*Cerebral angiography | * [[Magnetic resonance imaging]] (MRI) | ||
* Cerebral angiography | |||
===History and physical examination=== | |||
For laypersons, the Cincinnati Prehospital Stroke Scale (CPSS) is a [[clinical prediction rule]] that can diagnose stroke when any facial droop, arm drift, and speech. The accuracy is:<ref name="pmid15625998">{{cite journal |author=Liferidge AT, Brice JH, Overby BA, Evenson KR |title=Ability of laypersons to use the Cincinnati Prehospital Stroke Scale |journal=Prehosp Emerg Care |volume=8 |issue=4 |pages=384–7 |year=2004 |pmid=15625998 |doi= |url= |issn=}}</ref><ref name="pmid9332632">{{cite journal |author=Kothari R, Hall K, Brott T, Broderick J |title=Early stroke recognition: developing an out-of-hospital NIH Stroke Scale |journal=Acad Emerg Med |volume=4 |issue=10 |pages=986–90 |year=1997 |month=October |pmid=9332632 |doi= |url= |issn=}}</ref> | |||
* [[sensitivity (tests)|sensitivity]] = 94% to 100% | |||
* [[specificity (tests)|specificity]] = 83% to 88% | |||
The Face Arm Speech Test (FAST) scale is the same as the CPSS except speech is assessed informally without the patient having to repeat a sentence:<ref name="pmid21402744">{{cite journal| author=Whiteley WN, Wardlaw JM, Dennis MS, Sandercock PA| title=Clinical scores for the identification of stroke and transient ischaemic attack in the emergency department: a cross-sectional study. | journal=J Neurol Neurosurg Psychiatry | year= 2011 | volume= 82 | issue= 9 | pages= 1006-10 | pmid=21402744 | doi=10.1136/jnnp.2010.235010 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21402744 }} </ref><ref name="pmid21402744">{{cite journal| author=Whiteley WN, Wardlaw JM, Dennis MS, Sandercock PA| title=Clinical scores for the identification of stroke and transient ischaemic attack in the emergency department: a cross-sectional study. | journal=J Neurol Neurosurg Psychiatry | year= 2011 | volume= 82 | issue= 9 | pages= 1006-10 | pmid=21402744 | doi=10.1136/jnnp.2010.235010 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21402744 }} </ref> | |||
* [[sensitivity (tests)|sensitivity]] = 81% | |||
* [[specificity (tests)|specificity]] = 93% | |||
The National Institutes of Health Stroke Scale (NIHSS) is available.<ref name="urlNIH Stroke Scale Training: National Institute of Neurological Disorders and Stroke (NINDS)">{{cite web |url=http://www.ninds.nih.gov/doctors/stroke_scale_training.htm |title=NIH Stroke Scale Training: National Institute of Neurological Disorders and Stroke (NINDS) |author=Anonymous |authorlink= |coauthors= |date= |format= |work= |publisher=National Institute of Neurological Disorders and Stroke |pages= |language=English |archiveurl= |archivedate= |quote= |accessdate=2008-08-19}}</ref> Scores <=5 for patients with posterior circulation stroke and <=8 for anterior circulation stroke have a [[sensitivity (tests)|sensitivity]] of about 80% for predicting lack of independent living after 2 -3 months. | |||
For [[health care provider]]s, a [[systematic review]] by the [http://www.sgim.org/clinexam-rce.cfm Rational Clinical Examination] found that acute facial paresis, arm drift, or abnormal speech are the best findings <ref name="pmid15900010">{{cite journal |author=Goldstein L, Simel D |title=Is this patient having a stroke? |journal=JAMA |volume=293 |issue=19 |pages=2391-402 |year=2005 |id=PMID 15900010 | doi=10.1001/jama.296.16.2012 | url=http://jama.ama-assn.org/cgi/content/full/296/16/2012}}</ref>. | |||
Regarding distinction of patients with [[intracerebral hemorrhage]], most all patients will have one of:<ref name="pmid19687023">{{cite journal| author=Lovelock CE, Redgrave JN, Briley D, Rothwell PM| title=The SCAN rule: a clinical rule to reduce CT misdiagnosis of intracerebral haemorrhage in minor stroke. | journal=J Neurol Neurosurg Psychiatry | year= 2010 | volume= 81 | issue= 3 | pages= 271-5 | pmid=19687023 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19687023 | doi=10.1136/jnnp.2008.169227 }} </ref> | |||
* blood pressure 180/110 mm Hg | |||
* confusion | |||
* previous use of [[anticoagulant]]s | |||
* nausea or vomiting | |||
===Imaging=== | |||
{| class="wikitable" align="right" | |||
|+ [[Diagnostic imaging]] of acute stroke.<ref name="pmid19821415">{{cite journal| author=Brazzelli M, Sandercock PA, Chappell FM, Celani MG, Righetti E, Arestis N et al.| title=Magnetic resonance imaging versus computed tomography for detection of acute vascular lesions in patients presenting with stroke symptoms. | journal=Cochrane Database Syst Rev | year= 2009 | volume= | issue= 4 | pages= CD007424 | pmid=19821415 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=19821415 | doi=10.1002/14651858.CD007424.pub2 }}</ref><ref name="pmid17258669">{{cite journal |author=Chalela J, Kidwell C, Nentwich L, Luby M, Butman J, Demchuk A, Hill M, Patronas N, Latour L, Warach S |title=Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison |journal=Lancet |volume=369 |issue=9558 |pages=293-8 |year=2007 |id=PMID 17258669}}</ref> | |||
! rowspan="2"| !! colspan="2"|Ischemic stroke<ref name="pmid19821415"/>!! colspan="2"|Hemorrhagic stroke<ref name="pmid17258669"/> | |||
|- | |||
![[Sensitivity and specificity|Sensitivity]]!![[Sensitivity and specificity|Specificity]]!![[Sensitivity and specificity|Sensitivity]]!![[Sensitivity and specificity|Specificity]] | |||
|- | |||
| [[magnetic resonance imaging|MRI]] || 99%<br/> ([[Confidence interval|95% CI]] 0.23 to 1.00)|| 92%|| 81%|| 100% | |||
|- | |||
| [[X-ray computed tomography|CT scan]]|| 39%<br/>([[Confidence interval|95% CI]] 0.16 to 0.69)|| 100%|| 89%<sup>†</sup>|| 100%<sup>†</sup> | |||
|- | |||
|colspan="5"| † Without contrast enhancement | |||
|} | |||
[[Clinical practice guideline]]s recommend [[diffusion-weighted magnetic resonance imaging]] over perfusion weighted imaging ([[magnetic resonance angiography]]).<ref name="pmid20625171">{{cite journal| author=Schellinger PD, Bryan RN, Caplan LR, Detre JA, Edelman RR, Jaigobin C et al.| title=Evidence-based guideline: The role of diffusion and perfusion MRI for the diagnosis of acute ischemic stroke: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. | journal=Neurology | year= 2010 | volume= 75 | issue= 2 | pages= 177-85 | pmid=20625171 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20625171 | doi=10.1212/WNL.0b013e3181e7c9dd | pmc=PMC2905927 }} </ref> | |||
There is much variation in reports of the accuracy of diagnostic imagining according to a [[systematic review]] by the [[Cochrane Collaboration]] of [[diagnostic imaging]] with [[magnetic resonance imaging]] (MRI), especially [[diffusion magnetic resonance imaging]], and [[X-ray computed tomography]] (CT scan) within 12 hours of onset of symptoms (see table).<ref name="pmid19821415">{{cite journal| author=Brazzelli M, Sandercock PA, Chappell FM, Celani MG, Righetti E, Arestis N et al.| title=Magnetic resonance imaging versus computed tomography for detection of acute vascular lesions in patients presenting with stroke symptoms. | journal=Cochrane Database Syst Rev | year= 2009 | volume= | issue= 4 | pages= CD007424 | pmid=19821415 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=19821415 | doi=10.1002/14651858.CD007424.pub2 }}</ref><ref name="pmid15494579">{{cite journal| author=Kidwell CS, Chalela JA, Saver JL, Starkman S, Hill MD, Demchuk AM et al.| title=Comparison of MRI and CT for detection of acute intracerebral hemorrhage. | journal=JAMA | year= 2004 | volume= 292 | issue= 15 | pages= 1823-30 | pmid=15494579 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=15494579 | doi=10.1001/jama.292.15.1823 }} </ref> | |||
CT scan is more likely to show [[intracranial hemorrhage]] if one of severe hypertension (180/110 mm Hg), confusion, anticoagulation, nausea and vomiting are present (mnemonic is 'SCAN').<ref name="pmid19687023"/> | |||
===Cardiac monitoring=== | |||
Extended cardiac monitoring with either Holter monitoring or event loop recording may detect paroxysmal atrial fibrillation or flutter in about one patient in twenty.<ref name="pmid17901394">{{cite journal |author=Liao J, Khalid Z, Scallan C, Morillo C, O'Donnell M |title=Noninvasive cardiac monitoring for detecting paroxysmal atrial fibrillation or flutter after acute ischemic stroke: a systematic review |journal=Stroke |volume=38 |issue=11 |pages=2935–40 |year=2007 |pmid=17901394 |doi=10.1161/STROKEAHA.106.478685 |issn=}}</ref> | |||
==Treatment== | ==Treatment== | ||
Stroke is a '''medical emergency'''. Permanent neurologic damage or death can sometimes be avoided, but only if stroke is promptly diagnosed and treated. | Stroke is a '''medical emergency'''. Permanent neurologic damage or death can sometimes be avoided, but only if stroke is promptly diagnosed and treated. Stroke care may be best in hospital wards that are specifically for treating patients with strokes.<ref name="pmid17943737">{{cite journal |author= |title=Organised inpatient (stroke unit) care for stroke |journal=Cochrane Database Syst Rev |volume= |issue=4 |pages=CD000197 |year=2007 |pmid=17943737 |doi=10.1002/14651858.CD000197.pub2 |issn=}}</ref> | ||
=== | ===Thrombolytic therapy=== | ||
Presentation to a specialized stroke center | Presentation to a specialized stroke center early after the start of symptoms may allow for the reversal of the stroke with [[thrombolytic therapy]]. Thrombolytic therapy is the administration by clot-dissolving medications, or ''thrombolytics''. [[Tissue Plasminogen Activator]] (tPA) is the usual agent. Studies have shown that tPA given within 6 hours of the onset of stroke symptoms significantly reduces death and dependency, but there is a significant risk of bleeding, especially intracranial hemorrhage. If given within 3 hours, outcomes are improved, and risk is reduced.<ref>Gregory W. Albers, MD; Wayne M. Clark, MD; Kenneth P. Madden, MD, PhD Scott A. Hamilton, PhD.ATLANTIS Trial:Results for Patients Treated Within 3 Hours of Stroke Onset 2002;33:493</ref><ref>Joanna Wardlaw, Eivind Berge, Gergory delZoppo and Takenori Yamaguchi. Thrombolysis for acute ischemic stroke. Stroke. 2004;35:2914-2915.</ref> | ||
For patients who have had symptoms for less than 3 hours, recommendations by the American Heart Association for using [[Tissue Plasminogen Activator]]are available.<ref name="pmid17431204">{{cite journal |author=Adams HP, del Zoppo G, Alberts MJ, ''et al.'' |title=Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists |journal=Stroke |volume=38 |issue=5 |pages=1655–711 |year=2007 |month=May |pmid=17431204 |doi=10.1161/STROKEAHA.107.181486 |url=http://stroke.ahajournals.org/cgi/pmidlookup?view=long&pmid=17431204 |issn=}}</ref> | |||
For patients who have had symptoms for 3 to 4.5 hours, recommendations by the American Heart Association for using [[Tissue Plasminogen Activator]] include the following additional exclusion criteria:<ref name="pmid19478221">{{cite journal |author=Del Zoppo GJ, Saver JL, Jauch EC, Adams HP |title=Expansion of the Time Window for Treatment of Acute Ischemic Stroke With Intravenous Tissue Plasminogen Activator. A Science Advisory From the American Heart Association/American Stroke Association |journal=Stroke |volume= |issue= |pages= |year=2009 |month=May |pmid=19478221 |doi=10.1161/STROKEAHA.109.192535 |url= |issn=}}</ref> | |||
* Patients older than 80 years | |||
* Patients taking oral [[anticoagulation]] | |||
* Patients with a baseline National Institutes of Health [http://www.ninds.nih.gov/disorders/stroke/strokescales.htm Stroke Scale] score > 25 | |||
* Patients with both a history of stroke and [[diabetes]] | |||
[[Ultrasonic therapy]] has been used to enhance [[thrombolytic therapy]] therapy for stroke.<ref name="pmid20044531">{{cite journal| author=Tsivgoulis G, Eggers J, Ribo M, Perren F, Saqqur M, Rubiera M et al.| title=Safety and efficacy of ultrasound-enhanced thrombolysis: a comprehensive review and meta-analysis of randomized and nonrandomized studies. | journal=Stroke | year= 2010 | volume= 41 | issue= 2 | pages= 280-7 | pmid=20044531 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20044531 | doi=10.1161/STROKEAHA.109.563304 }} </ref> | |||
===Angioplasty=== | |||
"Overall, intervention results in a significant increase in the proportion of patients with a favourable outcome, despite a significant increase in intracranial haemorrhage" according to a [[meta-analysis]] by the [[Cochrane Collaboration]]. <ref name="pmid20927761">{{cite journal| author=O'Rourke K, Berge E, Walsh CD, Kelly PJ| title=Percutaneous vascular interventions for acute ischaemic stroke. | journal=Cochrane Database Syst Rev | year= 2010 | volume= 10 | issue= | pages= CD007574 | pmid=20927761 | doi=10.1002/14651858.CD007574.pub2 }} </ref> | |||
==Complications== | |||
Seizures may occur, especially within the first week:<ref name="pmid21975208">{{cite journal| author=Beghi E, D'Alessandro R, Beretta S, Consoli D, Crespi V, Delaj L et al.| title=Incidence and predictors of acute symptomatic seizures after stroke. | journal=Neurology | year= 2011 | volume= 77 | issue= 20 | pages= 1785-93 | pmid=21975208 | doi=10.1212/WNL.0b013e3182364878 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21975208 }} </ref> | |||
by presence of hemorrhage: | |||
* hemorrhagic strokes 16% | |||
* ischemic strokes 4% | |||
or by location: | |||
* cortical strokes 19% | |||
* noncortical strokes 10% | |||
==Prognosis== | |||
A [[meta-analysis]] calculated that the chance of recurrent stroke after an initial stroke is:<ref name="pmid21454819">{{cite journal| author=Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP| title=Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. | journal=Stroke | year= 2011 | volume= 42 | issue= 5 | pages= 1489-94 | pmid=21454819 | doi=10.1161/STROKEAHA.110.602615 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21454819 }} </ref> | |||
* 3.1% (95% CI, 1.7-4.4) at 30 days | |||
* 11.1% (95% CI, 9.0-13.3) at 1 year | |||
* 26.4% (95% CI, 20.1-32.8) at 5 years | |||
* 39.2% (95% CI, 27.2-51.2) at 10 years | |||
[[Clinical prediction rule]]s are available to guide prognosis for recovery of function<ref name="pmid18403738">{{cite journal |author=König IR, Ziegler A, Bluhmki E, ''et al'' |title=Predicting long-term outcome after acute ischemic stroke: a simple index works in patients from controlled clinical trials |journal=Stroke |volume=39 |issue=6 |pages=1821–6 |year=2008 |month=June |pmid=18403738 |doi=10.1161/STROKEAHA.107.505867 |url=http://stroke.ahajournals.org/cgi/pmidlookup?view=long&pmid=18403738 |issn=}}</ref> and recurrence<ref name="pmid19023098">{{cite journal |author=Weimar C, Diener HC, Alberts MJ, ''et al'' |title=The Essen stroke risk score predicts recurrent cardiovascular events: a validation within the REduction of Atherothrombosis for Continued Health (REACH) registry |journal=Stroke |volume=40 |issue=2 |pages=350–4 |year=2009 |month=February |pmid=19023098 |doi=10.1161/STROKEAHA.108.521419 |url=http://stroke.ahajournals.org/cgi/pmidlookup?view=long&pmid=19023098 |issn=}}</ref><ref name="pmid18849093">{{cite journal |author=Shah KH, Metz HA, Edlow JA |title=Clinical prediction rules to stratify short-term risk of stroke among patients diagnosed in the emergency department with a transient ischemic attack |journal=Ann Emerg Med |volume=53 |issue=5 |pages=662–73 |year=2009 |month=May |pmid=18849093 |doi=10.1016/j.annemergmed.2008.08.004 |url=http://linkinghub.elsevier.com/retrieve/pii/S0196-0644(08)01588-6 |issn=}}</ref> One clinical prediction rule is online at http://www.nmr.mgh.harvard.edu/RRE/.<ref name="pmid20018608">{{cite journal| author=Ay H, Gungor L, Arsava EM, Rosand J, Vangel M, Benner T et al.| title=A score to predict early risk of recurrence after ischemic stroke. | journal=Neurology | year= 2010 | volume= 74 | issue= 2 | pages= 128-35 | pmid=20018608 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20018608 | doi=10.1212/WNL.0b013e3181ca9cff | pmc=PMC2809031 }} </ref> | |||
Half of early recurrences occur within the first 24 hours.<ref name="pmid19487652">{{cite journal |author=Chandratheva A, Mehta Z, Geraghty OC, Marquardt L, Rothwell PM |title=Population-based study of risk and predictors of stroke in the first few hours after a TIA |journal=Neurology |volume=72 |issue=22 |pages=1941–7 |year=2009 |month=June |pmid=19487652 |doi=10.1212/WNL.0b013e3181a826ad |url= |issn=}}</ref> | |||
==Prevention== | ==Prevention== | ||
===Primary prevention=== | |||
Prevention of stroke involves reducing modifiable risk factors, and falls broadly into two categories: prevention of first stroke (primary prevention), and prevention of further strokes (secondary prevention). Also, some risk factors are ''modifiable'' (e.g. smoking), and some are not (e.g. age). Prevention, especially secondary prevention, involves certain medications. | Prevention of stroke involves reducing modifiable risk factors, and falls broadly into two categories: prevention of first stroke (primary prevention), and prevention of further strokes (secondary prevention). Also, some risk factors are ''modifiable'' (e.g. smoking), and some are not (e.g. age). Prevention, especially secondary prevention, involves certain medications. | ||
====Risk factor reduction==== | ====Risk factor reduction==== | ||
| Line 111: | Line 205: | ||
*HMG-CoA reductase inhibitors (Statins) | *HMG-CoA reductase inhibitors (Statins) | ||
*Angiogensin converting enzyme (ACE) inhibitors | *Angiogensin converting enzyme (ACE) inhibitors | ||
====Surgery==== | |||
[[Endarterectomy]], when the perioperative stroke or death is 3%, may reduce rate of stroke at 10 years according to a [[randomized controlled trial]].<ref name="pmid20870099">{{cite journal| author=Halliday A, Harrison M, Hayter E, Kong X, Mansfield A, Marro J et al.| title=10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (ACST-1): a multicentre randomised trial. | journal=Lancet | year= 2010 | volume= 376 | issue= 9746 | pages= 1074-84 | pmid=20870099 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20870099 | doi=10.1016/S0140-6736(10)61197-X }} </ref> | |||
===Secondary prevention=== | |||
Secondary prevention refers to preventing a second stroke in a patient who has had an initial stroke or TIA. | |||
====Medications==== | |||
[[Clopidogrel]] monotherapy has small benefit over aspirin<ref name="pmid8918275">{{cite journal |author= |title=A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee |journal=Lancet |volume=348 |issue=9038 |pages=1329–39 |year=1996 |month=November |pmid=8918275 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0140673696094573 |issn=}}</ref> and clopidogrel monotheray or combined with 75 mg [[aspirin]] to be similar to aspirin alone; however, but clopidogrel monotherapy reduces bleeding.<ref name="pmid15276392">{{cite journal |author=Diener HC, Bogousslavsky J, Brass LM, ''et al'' |title=Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial |journal=Lancet |volume=364 |issue=9431 |pages=331–7 |year=2004 |pmid=15276392 |doi=10.1016/S0140-6736(04)16721-4 |url=http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(04)16721-4 |issn=}}</ref> | |||
Regarding the combination of [[aspirin]] plus [[dipyridamole]]: | |||
* "Combination of [[aspirin]] plus [[dipyridamole]] is more effective than aspirin alone in preventing stroke and other serious vascular events in patients with minor stroke and TIAs" according to a [[meta-analysis]].<ref name="pmid18323511">{{cite journal |author=Verro P, Gorelick PB, Nguyen D |title=Aspirin plus dipyridamole versus aspirin for prevention of vascular events after stroke or TIA: a meta-analysis |journal=Stroke |volume=39 |issue=4 |pages=1358-63 |year=2008 |pmid=18323511 |doi=10.1161/STROKEAHA.107.496281 |url=http://stroke.ahajournals.org/cgi/pmidlookup?view=long&pmid=18323511}}</ref> This was largely based on the ESPIRT [[randomized controlled trial]].<ref name="pmid16714187">{{cite journal |author=Halkes PH, van Gijn J, Kappelle LJ, Koudstaal PJ, Algra A |title=Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial |journal=Lancet |volume=367 |issue=9523 |pages=1665–73 |year=2006 |month=May |pmid=16714187 |doi=10.1016/S0140-6736(06)68734-5 |url=http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(06)68734-5 |issn=}}</ref> | |||
* Clopidogrel may have similar benefit to the combination of [[aspirin]] plus [[dipyridamole]] according to the PRoFESS [[randomized controlled trial]].<ref name="pmid18753638">{{cite journal |author=Sacco RL, Diener HC, Yusuf S, ''et al'' |title=Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke |journal=N. Engl. J. Med. |volume=359 |issue=12 |pages=1238–51 |year=2008 |month=September |pmid=18753638 |doi=10.1056/NEJMoa0805002 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=18753638&promo=ONFLNS19 |issn= |accessdate=2008-12-10}}</ref> An accompanying editorial illustrated the impact of the PRoFESS trial on the earlier [[network meta-analysis]] that was contradictory ([http://content.nejm.org/content/vol0/issue2008/images/large/NEJMe0806806f1.jpeg figure from editorial]).<ref name="pmid18753641">{{cite journal |author=Kent DM, Thaler DE |title=Stroke Prevention -- Insights from Incoherence |journal=N. Engl. J. Med. |volume= |issue= |pages= |year=2008 |month=August |pmid=18753641 |doi=10.1056/NEJMe0806806 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=18753641&promo=ONFLNS19 |issn=}}</ref> In the network meta-analysis, combined aspirin and dipyridamole may be better than clopidogrel; however, the lead author received lecture fees and travel support from [[Boehringer Ingelheim]], the manufacturer of combined aspirin and dipyridamole.<ref name="pmid18349026">{{cite journal |author=Thijs V, Lemmens R, Fieuws S |title=Network meta-analysis: simultaneous meta-analysis of common antiplatelet regimens after transient ischaemic attack or stroke |journal=Eur. Heart J. |volume=29 |issue=9 |pages=1086–92 |year=2008 |month=May |pmid=18349026 |doi=10.1093/eurheartj/ehn106 |url=http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=18349026 |issn=}}</ref> | |||
====Stents==== | |||
"Stenting for symptomatic carotid stenosis should be avoided in older patients (age ≥70 years), but might be as safe as endarterectomy in younger patients" according to a [[meta-analysis]]. <ref name="pmid20832852">{{cite journal| author=Carotid Stenting Trialists' Collaboration. Bonati LH, Dobson J, Algra A, Branchereau A, Chatellier G et al.| title=Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data. | journal=Lancet | year= 2010 | volume= 376 | issue= 9746 | pages= 1062-73 | pmid=20832852 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20832852 | doi=10.1016/S0140-6736(10)61009-4 }} </ref> | |||
Stents have less short term effect, but similar intermediate term (1-4 years) effect as [[carotid endarterectomy]] according to an older [[meta-analysis]].<ref name="pmid20154049">{{cite journal| author=Meier P, Knapp G, Tamhane U, Chaturvedi S, Gurm HS| title=Short term and intermediate term comparison of endarterectomy versus stenting for carotid artery stenosis: systematic review and meta-analysis of randomised controlled clinical trials. | journal=BMJ | year= 2010 | volume= 340 | issue= | pages= c467 | pmid=20154049 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&email=badgett@uthscdsa.edu&retmode=ref&cmd=prlinks&id=20154049 | doi=10.1136/bmj.c467 }}</ref> | |||
Specific [[randomized controlled trial]]s have found: | |||
* Increased in a combined outcome of stroke, death, or procedural myocardial infarction over the first 4 months with stenting.<ref name="pmid20189239">{{cite journal| author=International Carotid Stenting Study investigators. Ederle J, Dobson J, Featherstone RL, Bonati LH, van der Worp HB et al.| title=Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (International Carotid Stenting Study): an interim analysis of a randomised controlled trial. | journal=Lancet | year= 2010 | volume= 375 | issue= 9719 | pages= 985-97 | pmid=20189239 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20189239 | doi=10.1016/S0140-6736(10)60239-5 }} </ref> | |||
* Similar results for the two procedures over four years.<ref name="pmid20505173">{{cite journal| author=Brott TG, Hobson RW, Howard G, Roubin GS, Clark WM, Brooks W et al.| title=Stenting versus endarterectomy for treatment of carotid-artery stenosis. | journal=N Engl J Med | year= 2010 | volume= 363 | issue= 1 | pages= 11-23 | pmid=20505173 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20505173 | doi=10.1056/NEJMoa0912321 }} </ref> | |||
<!--<ref name="pmid19182080">{{cite journal |author=Brekenfeld C, Schroth G, Mattle HP, ''et al.'' |title=Stent placement in acute cerebral artery occlusion: use of a self-expandable intracranial stent for acute stroke treatment |journal=Stroke |volume=40 |issue=3 |pages=847–52 |year=2009 |month=March |pmid=19182080 |doi=10.1161/STROKEAHA.108.533810 |url=http://stroke.ahajournals.org/cgi/pmidlookup?view=long&pmid=19182080 |issn=}}</ref>--> | |||
==References== | ==References== | ||
<references | <small> | ||
<references> | |||
</references> | |||
[[Category: | </small>[[Category:Suggestion Bot Tag]] | ||
Latest revision as of 16:01, 22 October 2024
A stroke (syn. Cerebral Vascular Accident or "CVA") is a sudden, often focal, loss of brain function. "Cerebral vascular accident" summarizes features of a stroke: (1) "cerebral" (brain) (2) "vascular" (blood supply) and (3) "accident" indicates that this is a rapid and detrimental event. Although most strokes in people do involve the higher centers of the brain that are located in the cerebral hemispheres; the word cerebral is not strictly accurate, as some strokes can involve only the lower portions of the brain, like the medulla oblongata or other areas of the brain stem. Most stroke experts prefer the term "stroke" to "CVA", but both are used commonly to refer to this acquired neurological disorder. The term "brain attack" has been advocated for use in the United States for stroke, just as the term "heart attack" is used for myocardial infarction, to reinforce the idea that urgent treatment of developing stroke is essential.
Many hospitals have multidisciplinary "stroke teams" specifically for swift treatment of stroke. While an emergency physician may first see the patient, neurologists, neurosurgeons and interventional radiologists may quickly become involved. The patient is apt to need both immediate critical care and long term rehabilitation.
For survivors of stroke, treatment is important in three distinct phases after the incident. Immediate treatment in the minutes and hours after the first signs of a stroke can sometimes change the course of the acute event by removing factors (like an embolus or extreme hypertension) that will otherwise promote greater and greater injury. Treatment after the acute stroke rehabilitation therapy can offer the best hope of maximal recovery for most patients by aiding the person's ability to use their surviving brain to take over some of the functions that damaged tissues cannot manage, and long term therapy can help reduce the underlying risks of another stroke.
Epidemiology
Stroke is one of the leading causes of long term disability, and of death, in the developed world. Approximately 700,000 Americans per year experience a stroke. It is the third leading cause of death and the leading cause of long-term adult disability in the United States.[1] On average, a stroke occurs every 45 seconds and someone dies from a stroke every 3 minutes.[2][3]
Asymptomatic infarctions, usually lacunar, are present in 7% of MRI scans; 2% of scans detect incidental intracranial aneurysms.[4]
Risk factors for stroke include atherosclerosis, advanced age, hypertension (high blood pressure), diabetes mellitus, high cholesterol, cigarette smoking, atrial fibrillation, migraine headaches[5], ethnic identity, and some blood clotting disorders.
Causes
There are many different causes of stroke, but whenever a stroke occurs, there has been an interruption of the normal blood supply to brain cells that has gone on long enough to cause death to at least some of them. If the loss is so brief that the brain tissue can quickly recover, and does not die, then a Transient Ischemic Attack (TIA) has occurred, rather than a stroke.The symptoms and signs of a stroke are highly dependent upon the number of cells that are affected, and exactly where these cells are located in the brain. Accordingly, strokes can have many different clinical presentations - ranging from deep coma with the loss of the ability to breathe; to very limited deficits in the ability to move a part of the body, or changes in sensory perception like partial blindness from a restriction in visual field, without any associated problems with movement.
The interruption of blood circulation generally comes about either because (1) blood flow is stopped (occluded) within the blood vessel, or because (2) the blood vessel ruptures (hemorrhages). In either case, the vessel no longer serves to supply the brain cells with nutrients and oxygen. Hemorrhages hurt the brain in ways besides starving cells, the break in the vessels from a hemmorrhage floods the blood it carries into an expanding clot that also causes damage from excessive pressure.
Ordinarily, at least some brain tissue is injured by a stroke - yet not killed. The injury to these cells is reversible. That's one reason why the amount of recovery during the initial time period after a stroke is difficult to predict, and also why treatment at that time can influence the course of recovery. If the stroke patient survives the stroke, some brain cells may actually recover in time if the injury was not too great. Since the central nervous system, even in older adults, has at least some ability to adjust to loss of (plasticity), such that other areas of the brain can often take over partial functions of the damaged areas, there may be more recovery of function over time for the patient, even once the damaged areas of the brain are no longer capable of any additional recovery of injured brain cells.
Anatomy
The brain is made out of nerve cells and supporting cells, it is covered by protective layers and it is moistened by the constant circulation of a pristine fluid called "cerebrospinal fluid" (CSF).
Like all parts of the body, the brain has vessels that pump blood to it from the heart called arteries and vessels that collect the blood after circulating through the organ for return to the heart called veins. As in most organs of the body, the arteries to the brain carry blood loaded with oxygen and glucose (blood sugar) and the veins carry away blood that has delivered these vital supplies to the cells of the brain and had their waste products dumped in it.
There are special features of the vasculature to the brain that are protective since brain cells are more vulnerable to loss of oxygen and glucose than are the cells of any other portion of the body. One of these features is the circular design of the blood delivery system to the brain. This circle of arteries that joins blood pumped up from the front of the neck ( the carotid arteries) from blood pumped up from the back (the vertebral arteries). In most healthy young people, this system of blood flow is so good that even if one of the arteries is lost altogether (from an injury, for example), the others can make up for it and keep delivering a properly working circulation of fresh arterial blood, and no impairment to the brain cells occurs.
Classification of Strokes
This section aims to lay out the types of strokes so that the rest of the article is more easily understood. Strokes can be classified according to the mechanism of injury, and also according to the areas of the brain that are injured. Need to reorganize to have "classification", then specific types/subtypes.
Strokes can be classified as ischemic or hemorrhagic. In ischemic strokes, all or part of the brain is deprived of blood and oxygen, usually through the blockage of an artery. In hemorrhagic strokes, loss of blood supply plays a part, but the initial event is bleeding into the brain causing increased pressure on the brain, and irritation to brain tissue.
Ischemic strokes
The word ischemia indicates the loss of blood supply to tissues. When tissues are ischemic, they are generally pale and, if the ischemia persists long enough, become swollen and change further as cells swell and then die. The area of dead (also called necrotic) tissue that results from ischemia is called an infarct.
- Ischemic strokes make up about 87% of all strokes and can be due to blockage of a feeding artery by a clot or by generalized low blood flow (hypoperfusion), along with narrowed arteries. Lacunae, or small vessel ischemic strokes, are responsible for about 20% of all strokes and are common in hypertension and diabetes mellitus.
- Hemorrhagic strokes are usually classed as either intracerebral hemorrhage or subarachnoid hemorrhage.[6] Uncontrolled hypertension is a leading cause of hemorrhagic stroke. Weaknesses in brain arteries, (for example, intracranial aneurysms) can cause hemorrhagic strokes even when the pressure of the blood inside the arteries is not excessive. Because the brain is enclosed within a rigid structure (the skull), even a small amount of bleeding can cause a dramatic increase in pressure on the brain. This can lead to herniation, in which part of the brain is compressed through the base of the skull, causing rapid coma and death.
Atherosclerosis is responsible for the majority of ischemic strokes. The etiology of atherosclerosis-related strokes is very similar to that of heart attacks. An atherosclerotic plaque in a cerebral artery can gradually develop an associated thrombus or rupture suddenly causing a rapid occlusion, or the thrombus can break off and lodge in a vessel even deeper in the brain. "Thrombotic stroke" usually refers to in-situ thrombus, "embolic stroke" to thrombi that travel from distant sites.
Thrombotic Stroke
Thrombotic and thromboembolic strokes can originate in either large or small blood vessels, and are usually due to abnormalities in the vessel (most commonly atherosclerosis). Atheroembolism can occur within the cerebral circulation or can originate outside the cerebral circulation. One of the most important etiologies is carotid artery disease. Lacunae are also a subset of thrombotic stroke.
Embolic Stroke
Embolism of thrombi from outside the cerebral circulation are responsible for a large and important subset of ischemic strokes. In these cases a thrombus (blood clot) travels from its origin and lodges in a cerebral artery. Most of these strokes are of cardiac origin (Cardioembolic).
Cardioembolic Stroke
- Atrial fibrillation: The majority of embolic strokes originating in the heart are due to atrial fibrillation. In fact, about 16% of strokes are associated with atrial fibrillation, and the presence of atrial fibrillation increases stroke risk by about 5-11% per year, depending on other risk factors. [7]The relative stasis of blood in the left atrium leads to blood clot formation, and these clots can be expelled from the heart to enter the cerebral circulation.
- Mural thrombi: anything that causes blood flow in the heart to slow can cause thrombus formation. This includes thrombi formed in the atrial appendage and thrombi formed in the left ventricle in patients with heart failure.
- Valvular heart disease: this includes rheumatic heart disease, infective endocarditis, and presence of a prosthetic heart valve.
- Paradoxical embolism: this occurs primarily when a thrombosis elsewhere in the body breaks off, passing through a patent foramen ovale (PFO) into the left ventricle (especially if an atrial septal aneurysm is present), and then to the brain.[8]
Systemic hypoperfusion (Watershed stroke)
Systemic hypoperfusion is the reduction of blood flow to all parts of the body. It is most commonly due to various types of shock. Hypoxemia (low blood oxygen content) may precipitate the hypoperfusion. Because the reduction in blood flow is global, all parts of the brain may be affected, especially "watershed" areas --- border zone regions supplied by the major cerebral arteries. Blood flow to these areas does not necessarily stop, but instead it may lessen to the point where brain damage can occur.
Hemorrhagic stroke
A hemorrhagic stroke, or cerebral hemorrhage, is a form of stroke that occurs when a blood vessel in the brain ruptures or bleeds. There are two types of hemorrhagic stroke: intracerebral hemorrhage, and subarachnoid hemorrhage (SAH). Traumatic hemorrhage, including epidural hemorrhage, subdural hemorrhage, and some SAH are usually considered separately.
Intracerebral hemorrhage
Intracerebral hemorrhage (ICH) is bleeding directly into the brain tissue, forming a gradually enlarging hematoma (pool of blood). It generally occurs in small arteries or arterioles and is commonly due to hypertension, trauma, and vascular malformations. The hematoma enlarges until pressure from surrounding tissue limits its growth, or until it decompresses by emptying into the ventricular system. ICH has a mortality rate of 44 percent after 30 days, higher than ischemic stroke or even the very deadly subarachnoid hemorrhage.[9]
Subarachnoid hemorrhage
Subarachnoid hemorrhage (SAH) is bleeding into the cerebrospinal fluid (CSF) surrounding the brain. The two most common causes of SAH are rupture of intracranial aneurysm and bleeding from vascular malformations. Bleeding into the CSF from a ruptured aneurysm occurs very quickly, causing rapidly increased intracranial pressure. The initial bleed can be brief, but rebleeding is common. Death or deep coma ensues if the bleeding continues. SAH has a 37-45% mortality for patients 45 and older.[10][11] Intracranial aneurysm can be associated with other disorders, such as adult polycystic kidney disease.
Risk Factors
Many factors are generally agreed to cause a higher risk for a stroke.[12]
- Previous stroke
- Atherosclerosis: many of the risk factors listed below are also risk factors for atherosclerosis. Other marker for atherosclerosis include peripheral artery disease and coronary artery disease.
- Hypertension is the most powerful risk factor for ischemic stroke, and the primary risk factor for intracerebral hemorrhagic stroke. [13][14]
- Smoking: cigarette smoking significantly increases stroke risk, and the risk is dependent on the amount of smoking.[15] Cigar and pipe smoke also increase stroke risk but to a lesser degree.
- Transient Ischemic Attack: Occurrence of TIA is a strong risk factor for stroke. In one study, 5% of patients with TIA developed stroke within 2 days, 10% within 90 days.[16] TIA should be considered a medical emergency; rapid response reduces the risk of stroke.
- Atrial Fibrillation (AF): The average yearly risk for stroke in untreated AF is 5%, but can be as high as 12%.[17]
- Diabetes mellitus: Diabetes is a major stroke risk.[18]
- Age: the risk of stroke in adults increases significantly over the age of 55, and continues to increase thereafter.
- Ethnicity: African Americans have twice the risk of a first stroke as whites.
- Carotid stenosis (asymptomatic)
- Cocaine: cocaine use is a significant risk for stroke and heart attack.
- Blood disorders (e.g. sickle-cell disease, anti-cardiolipin syndrome)
- Estrogen: recent studies have found small but significant increase in stroke risk in women receiving hormone replacement therapy (HRT). In one large study, stroke risk was increase by 55%, which equates to 12 additional strokes per 10,000 person-years.[19] Oral contraceptive pills (OCPs) may confer some risk, especially when combined with other risks such as smoking, however the risk from the currently used low-dose OCPs is quite low.[20]
- Pregnancy: there is a small but significant increase in stroke risk during, and just after pregnancy.
Symptoms
The symptoms of stroke depend on what part of the brain is affected. A friend or family member may be the first to notice. Symptoms can include:
- Sudden numbness or weakness of the face, arm, or leg, especially one-sided
- Sudden confusion, trouble speaking, or trouble understanding
- Sudden trouble walking, dizziness, or loss of balance or coordination
- Sudden trouble seeing in 1 or both eyes
- Sudden severe headache
- Difficulty swallowing or drooling
Diagnosis
A stroke is diagnosed first by a medical professional taking a proper history and physical exam. However, 13% of suspected strokes may actually be a seizure, migraine headache, or conversion disorder.[21] Tests include:
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Cerebral angiography
History and physical examination
For laypersons, the Cincinnati Prehospital Stroke Scale (CPSS) is a clinical prediction rule that can diagnose stroke when any facial droop, arm drift, and speech. The accuracy is:[22][23]
- sensitivity = 94% to 100%
- specificity = 83% to 88%
The Face Arm Speech Test (FAST) scale is the same as the CPSS except speech is assessed informally without the patient having to repeat a sentence:[24][24]
- sensitivity = 81%
- specificity = 93%
The National Institutes of Health Stroke Scale (NIHSS) is available.[25] Scores <=5 for patients with posterior circulation stroke and <=8 for anterior circulation stroke have a sensitivity of about 80% for predicting lack of independent living after 2 -3 months.
For health care providers, a systematic review by the Rational Clinical Examination found that acute facial paresis, arm drift, or abnormal speech are the best findings [26].
Regarding distinction of patients with intracerebral hemorrhage, most all patients will have one of:[27]
- blood pressure 180/110 mm Hg
- confusion
- previous use of anticoagulants
- nausea or vomiting
Imaging
| Ischemic stroke[28] | Hemorrhagic stroke[29] | |||
|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | Specificity | |
| MRI | 99% (95% CI 0.23 to 1.00) |
92% | 81% | 100% |
| CT scan | 39% (95% CI 0.16 to 0.69) |
100% | 89%† | 100%† |
| † Without contrast enhancement | ||||
Clinical practice guidelines recommend diffusion-weighted magnetic resonance imaging over perfusion weighted imaging (magnetic resonance angiography).[30]
There is much variation in reports of the accuracy of diagnostic imagining according to a systematic review by the Cochrane Collaboration of diagnostic imaging with magnetic resonance imaging (MRI), especially diffusion magnetic resonance imaging, and X-ray computed tomography (CT scan) within 12 hours of onset of symptoms (see table).[28][31]
CT scan is more likely to show intracranial hemorrhage if one of severe hypertension (180/110 mm Hg), confusion, anticoagulation, nausea and vomiting are present (mnemonic is 'SCAN').[27]
Cardiac monitoring
Extended cardiac monitoring with either Holter monitoring or event loop recording may detect paroxysmal atrial fibrillation or flutter in about one patient in twenty.[32]
Treatment
Stroke is a medical emergency. Permanent neurologic damage or death can sometimes be avoided, but only if stroke is promptly diagnosed and treated. Stroke care may be best in hospital wards that are specifically for treating patients with strokes.[33]
Thrombolytic therapy
Presentation to a specialized stroke center early after the start of symptoms may allow for the reversal of the stroke with thrombolytic therapy. Thrombolytic therapy is the administration by clot-dissolving medications, or thrombolytics. Tissue Plasminogen Activator (tPA) is the usual agent. Studies have shown that tPA given within 6 hours of the onset of stroke symptoms significantly reduces death and dependency, but there is a significant risk of bleeding, especially intracranial hemorrhage. If given within 3 hours, outcomes are improved, and risk is reduced.[34][35]
For patients who have had symptoms for less than 3 hours, recommendations by the American Heart Association for using Tissue Plasminogen Activatorare available.[36]
For patients who have had symptoms for 3 to 4.5 hours, recommendations by the American Heart Association for using Tissue Plasminogen Activator include the following additional exclusion criteria:[37]
- Patients older than 80 years
- Patients taking oral anticoagulation
- Patients with a baseline National Institutes of Health Stroke Scale score > 25
- Patients with both a history of stroke and diabetes
Ultrasonic therapy has been used to enhance thrombolytic therapy therapy for stroke.[38]
Angioplasty
"Overall, intervention results in a significant increase in the proportion of patients with a favourable outcome, despite a significant increase in intracranial haemorrhage" according to a meta-analysis by the Cochrane Collaboration. [39]
Complications
Seizures may occur, especially within the first week:[40] by presence of hemorrhage:
- hemorrhagic strokes 16%
- ischemic strokes 4%
or by location:
- cortical strokes 19%
- noncortical strokes 10%
Prognosis
A meta-analysis calculated that the chance of recurrent stroke after an initial stroke is:[41]
- 3.1% (95% CI, 1.7-4.4) at 30 days
- 11.1% (95% CI, 9.0-13.3) at 1 year
- 26.4% (95% CI, 20.1-32.8) at 5 years
- 39.2% (95% CI, 27.2-51.2) at 10 years
Clinical prediction rules are available to guide prognosis for recovery of function[42] and recurrence[43][44] One clinical prediction rule is online at http://www.nmr.mgh.harvard.edu/RRE/.[45]
Half of early recurrences occur within the first 24 hours.[46]
Prevention
Primary prevention
Prevention of stroke involves reducing modifiable risk factors, and falls broadly into two categories: prevention of first stroke (primary prevention), and prevention of further strokes (secondary prevention). Also, some risk factors are modifiable (e.g. smoking), and some are not (e.g. age). Prevention, especially secondary prevention, involves certain medications.
Risk factor reduction
- Keeping blood pressure below 120/80 reduces the risk of both primary and recurrent stroke.[13][14]
- Quitting smoking decreases risk significantly 2 years after quitting cigarettes.[15]
- Transient ischemic attack (TIA) is a brief period of stroke symptoms, and is a warning sign of impending stroke. Seeking emergency medical attention reduces the risk of stroke after TIA.
- The risk of stroke due to atrial fibrillation can be significantly reduced with the use of oral anticoagulants (i.e. warfarin).[47][48]
- Diabetes is a major stroke risk factor. The role of good blood sugar control in the prevention of stroke in diabetics is still being investigated. Aggressive treatment of cholesterol and blood pressure in diabetics is essential. Certain medications help prevent strokes in diabetics.[49][50]
- High Cholesterol: treatment of high cholesterol and other blood lipid disorders reduces the rate of first stroke and recurrent stroke. [51]
Medications
- Aspirin
- Plavix
- Aggrenox
- Warfarin
- HMG-CoA reductase inhibitors (Statins)
- Angiogensin converting enzyme (ACE) inhibitors
Surgery
Endarterectomy, when the perioperative stroke or death is 3%, may reduce rate of stroke at 10 years according to a randomized controlled trial.[52]
Secondary prevention
Secondary prevention refers to preventing a second stroke in a patient who has had an initial stroke or TIA.
Medications
Clopidogrel monotherapy has small benefit over aspirin[53] and clopidogrel monotheray or combined with 75 mg aspirin to be similar to aspirin alone; however, but clopidogrel monotherapy reduces bleeding.[54]
Regarding the combination of aspirin plus dipyridamole:
- "Combination of aspirin plus dipyridamole is more effective than aspirin alone in preventing stroke and other serious vascular events in patients with minor stroke and TIAs" according to a meta-analysis.[55] This was largely based on the ESPIRT randomized controlled trial.[56]
- Clopidogrel may have similar benefit to the combination of aspirin plus dipyridamole according to the PRoFESS randomized controlled trial.[57] An accompanying editorial illustrated the impact of the PRoFESS trial on the earlier network meta-analysis that was contradictory (figure from editorial).[58] In the network meta-analysis, combined aspirin and dipyridamole may be better than clopidogrel; however, the lead author received lecture fees and travel support from Boehringer Ingelheim, the manufacturer of combined aspirin and dipyridamole.[59]
Stents
"Stenting for symptomatic carotid stenosis should be avoided in older patients (age ≥70 years), but might be as safe as endarterectomy in younger patients" according to a meta-analysis. [60]
Stents have less short term effect, but similar intermediate term (1-4 years) effect as carotid endarterectomy according to an older meta-analysis.[61]
Specific randomized controlled trials have found:
- Increased in a combined outcome of stroke, death, or procedural myocardial infarction over the first 4 months with stenting.[62]
- Similar results for the two procedures over four years.[63]
References
- ↑ Centers for Disease Control and Prevention (CDC). Prevalence of disabilities and associated health conditions among adults: United States, 1999. MMWR Morb Mortal Wkly Rep. 2001; 50: 120–125
- ↑ Circulation. 2007;115:e69-e171.
- ↑ http://circ.ahajournals.org/cgi/content/full/CIRCULATIONAHA.106.179918
- ↑ Vernooij MW et al. Incidental Findings on Brain MRI in the General Population. New Eng J Med 2007. http://content.nejm.org/cgi/content/abstract/357/18/1821
- ↑ Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T (2009). "Migraine and cardiovascular disease: systematic review and meta-analysis.". BMJ 339: b3914. DOI:10.1136/bmj.b3914. PMID 19861375. Research Blogging.
- ↑ Goldman: Cecil Textbook of Medicine, 22nd ed., Copyright © 2004 W. B. Saunders Company
- ↑ Robert G. Hart, MD Jonathan L. Halperin, MD. Atrial Fibrillation and Stroke Concepts and Controversies. Stroke. 2001;32:803.
- ↑ Handke M, Harloff A, Olschewski M, Hetzel A, Geibel A (2007). "Patent foramen ovale and cryptogenic stroke in older patients". N. Engl. J. Med. 357 (22): 2262–8. DOI:10.1056/NEJMoa071422. PMID 18046029. Research Blogging.
- ↑ Caplan LR (1992). "Intracerebral hemorrhage". Lancet 339 (8794): 656-8. PMID 1347346.
- ↑ El-Saed A, Kuller LH, Newman AB, Lopez O, Costantino J, McTigue K, Cushman M, Kronmal R. Geographic variations in stroke incidence and mortality among older populations in four US communities. Stroke. 2006; 37: 1975–1979.
- ↑ Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, Copper LS, Shahar E. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerotic Risk in Communities (ARIC) Cohort. Stroke. 1999; 30: 736–743
- ↑ Goldstein LB. Adams R. Alberts MJ. Appel LJ. Brass LM. Bushnell CD. Culebras A. DeGraba TJ. Gorelick PB. Guyton JR. Hart RG. Howard G. Kelly-Hayes M. Nixon JV. Sacco RL. American Heart Association. American Stroke Association Stroke Council. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 113(24):e873-923, 2006 Jun 20
- ↑ 13.0 13.1 ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial.Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).JAMA. 288(23):2981-97, 2002 Dec 18.
- ↑ 14.0 14.1 Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, Wolf PA. The lifetime risk of stroke: Estimates from the Framingham study. Stroke. 2006; 37: 345–350
- ↑ 15.0 15.1 Wolf PA, D’Agostino RB, Kannel WB, Bonita R, Belanger AJ. Cigarette smoking as a risk factor for stroke: the Framingham study. JAMA. 1988; 259: 1025–1029
- ↑ Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000; 284: 2901–2906
- ↑ Hylek E. M., Go A. S., Chang Y., Jensvold N. G., Henault L. E., Selby J. V., Singer D. E. N Engl J Med 2003; 349:1019-1026, Sep 11, 2003
- ↑ Stroke in Patients With Diabetes and Hypertension. Samy I. McFarlane, MD, MPH, Domenic A. Sica, MD, James R. Sowers, MD. J Clin Hypertens (Greenwich). 2005;7(5):286-292.
- ↑ Hendrix SL, Wassertheil-Smoller S, Johnson KC, Howard BV, Kooperberg C, Rossouw JE, Trevisan M, Aragaki A, Baird AE, Bray PF, Buring JE, Criqui MH, Herrington D, Lynch JK, Rapp SR, Torner J, WHI investigators. Effects of conjugated equine estrogen on stroke in the Women’s Health Initiative. Circulation. 2006; 113: 2425–2434
- ↑ Sasitorn Siritho, MD; Amanda G. Thrift, PhD; John J. McNeil, PhD; Roger X. You, PhD; Stephen M. Davis, MD Geoffrey A. Donnan, MD. Risk of Ischemic Stroke Among Users of the Oral Contraceptive Pill. The Melbourne Risk Factor Study (MERFS) Group. Stroke, Vol 22, 312-318
- ↑ Chernyshev OY, Martin-Schild S, Albright KC, Barreto A, Misra V, Acosta I et al. (2010). "Safety of tPA in stroke mimics and neuroimaging-negative cerebral ischemia.". Neurology 74 (17): 1340-5. DOI:10.1212/WNL.0b013e3181dad5a6. PMID 20335564. Research Blogging.
- ↑ Liferidge AT, Brice JH, Overby BA, Evenson KR (2004). "Ability of laypersons to use the Cincinnati Prehospital Stroke Scale". Prehosp Emerg Care 8 (4): 384–7. PMID 15625998. [e]
- ↑ Kothari R, Hall K, Brott T, Broderick J (October 1997). "Early stroke recognition: developing an out-of-hospital NIH Stroke Scale". Acad Emerg Med 4 (10): 986–90. PMID 9332632. [e]
- ↑ 24.0 24.1 Whiteley WN, Wardlaw JM, Dennis MS, Sandercock PA (2011). "Clinical scores for the identification of stroke and transient ischaemic attack in the emergency department: a cross-sectional study.". J Neurol Neurosurg Psychiatry 82 (9): 1006-10. DOI:10.1136/jnnp.2010.235010. PMID 21402744. Research Blogging.
- ↑ Anonymous. NIH Stroke Scale Training: National Institute of Neurological Disorders and Stroke (NINDS) (English). National Institute of Neurological Disorders and Stroke. Retrieved on 2008-08-19.
- ↑ Goldstein L, Simel D (2005). "Is this patient having a stroke?". JAMA 293 (19): 2391-402. DOI:10.1001/jama.296.16.2012. PMID 15900010. Research Blogging.
- ↑ 27.0 27.1 Lovelock CE, Redgrave JN, Briley D, Rothwell PM (2010). "The SCAN rule: a clinical rule to reduce CT misdiagnosis of intracerebral haemorrhage in minor stroke.". J Neurol Neurosurg Psychiatry 81 (3): 271-5. DOI:10.1136/jnnp.2008.169227. PMID 19687023. Research Blogging.
- ↑ 28.0 28.1 28.2 Brazzelli M, Sandercock PA, Chappell FM, Celani MG, Righetti E, Arestis N et al. (2009). "Magnetic resonance imaging versus computed tomography for detection of acute vascular lesions in patients presenting with stroke symptoms.". Cochrane Database Syst Rev (4): CD007424. DOI:10.1002/14651858.CD007424.pub2. PMID 19821415. Research Blogging.
- ↑ 29.0 29.1 Chalela J, Kidwell C, Nentwich L, Luby M, Butman J, Demchuk A, Hill M, Patronas N, Latour L, Warach S (2007). "Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison". Lancet 369 (9558): 293-8. PMID 17258669.
- ↑ Schellinger PD, Bryan RN, Caplan LR, Detre JA, Edelman RR, Jaigobin C et al. (2010). "Evidence-based guideline: The role of diffusion and perfusion MRI for the diagnosis of acute ischemic stroke: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology.". Neurology 75 (2): 177-85. DOI:10.1212/WNL.0b013e3181e7c9dd. PMID 20625171. PMC PMC2905927. Research Blogging.
- ↑ Kidwell CS, Chalela JA, Saver JL, Starkman S, Hill MD, Demchuk AM et al. (2004). "Comparison of MRI and CT for detection of acute intracerebral hemorrhage.". JAMA 292 (15): 1823-30. DOI:10.1001/jama.292.15.1823. PMID 15494579. Research Blogging.
- ↑ Liao J, Khalid Z, Scallan C, Morillo C, O'Donnell M (2007). "Noninvasive cardiac monitoring for detecting paroxysmal atrial fibrillation or flutter after acute ischemic stroke: a systematic review". Stroke 38 (11): 2935–40. DOI:10.1161/STROKEAHA.106.478685. PMID 17901394. Research Blogging.
- ↑ (2007) "Organised inpatient (stroke unit) care for stroke". Cochrane Database Syst Rev (4): CD000197. DOI:10.1002/14651858.CD000197.pub2. PMID 17943737. Research Blogging.
- ↑ Gregory W. Albers, MD; Wayne M. Clark, MD; Kenneth P. Madden, MD, PhD Scott A. Hamilton, PhD.ATLANTIS Trial:Results for Patients Treated Within 3 Hours of Stroke Onset 2002;33:493
- ↑ Joanna Wardlaw, Eivind Berge, Gergory delZoppo and Takenori Yamaguchi. Thrombolysis for acute ischemic stroke. Stroke. 2004;35:2914-2915.
- ↑ Adams HP, del Zoppo G, Alberts MJ, et al. (May 2007). "Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists". Stroke 38 (5): 1655–711. DOI:10.1161/STROKEAHA.107.181486. PMID 17431204. Research Blogging.
- ↑ Del Zoppo GJ, Saver JL, Jauch EC, Adams HP (May 2009). "Expansion of the Time Window for Treatment of Acute Ischemic Stroke With Intravenous Tissue Plasminogen Activator. A Science Advisory From the American Heart Association/American Stroke Association". Stroke. DOI:10.1161/STROKEAHA.109.192535. PMID 19478221. Research Blogging.
- ↑ Tsivgoulis G, Eggers J, Ribo M, Perren F, Saqqur M, Rubiera M et al. (2010). "Safety and efficacy of ultrasound-enhanced thrombolysis: a comprehensive review and meta-analysis of randomized and nonrandomized studies.". Stroke 41 (2): 280-7. DOI:10.1161/STROKEAHA.109.563304. PMID 20044531. Research Blogging.
- ↑ O'Rourke K, Berge E, Walsh CD, Kelly PJ (2010). "Percutaneous vascular interventions for acute ischaemic stroke.". Cochrane Database Syst Rev 10: CD007574. DOI:10.1002/14651858.CD007574.pub2. PMID 20927761. Research Blogging.
- ↑ Beghi E, D'Alessandro R, Beretta S, Consoli D, Crespi V, Delaj L et al. (2011). "Incidence and predictors of acute symptomatic seizures after stroke.". Neurology 77 (20): 1785-93. DOI:10.1212/WNL.0b013e3182364878. PMID 21975208. Research Blogging.
- ↑ Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP (2011). "Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis.". Stroke 42 (5): 1489-94. DOI:10.1161/STROKEAHA.110.602615. PMID 21454819. Research Blogging.
- ↑ König IR, Ziegler A, Bluhmki E, et al (June 2008). "Predicting long-term outcome after acute ischemic stroke: a simple index works in patients from controlled clinical trials". Stroke 39 (6): 1821–6. DOI:10.1161/STROKEAHA.107.505867. PMID 18403738. Research Blogging.
- ↑ Weimar C, Diener HC, Alberts MJ, et al (February 2009). "The Essen stroke risk score predicts recurrent cardiovascular events: a validation within the REduction of Atherothrombosis for Continued Health (REACH) registry". Stroke 40 (2): 350–4. DOI:10.1161/STROKEAHA.108.521419. PMID 19023098. Research Blogging.
- ↑ Shah KH, Metz HA, Edlow JA (May 2009). "Clinical prediction rules to stratify short-term risk of stroke among patients diagnosed in the emergency department with a transient ischemic attack". Ann Emerg Med 53 (5): 662–73. DOI:10.1016/j.annemergmed.2008.08.004. PMID 18849093. Research Blogging.
- ↑ Ay H, Gungor L, Arsava EM, Rosand J, Vangel M, Benner T et al. (2010). "A score to predict early risk of recurrence after ischemic stroke.". Neurology 74 (2): 128-35. DOI:10.1212/WNL.0b013e3181ca9cff. PMID 20018608. PMC PMC2809031. Research Blogging.
- ↑ Chandratheva A, Mehta Z, Geraghty OC, Marquardt L, Rothwell PM (June 2009). "Population-based study of risk and predictors of stroke in the first few hours after a TIA". Neurology 72 (22): 1941–7. DOI:10.1212/WNL.0b013e3181a826ad. PMID 19487652. Research Blogging.
- ↑ Stroke Prevention in Atrial Fibrillation Investigators. Stroke prevention in atrial fibrillation study: Final results. Circulation 1991; 84:527. Aspirin alone only minimally reduces stroke risk.
- ↑ Petersen, P, Boysen, G, Godtfredsen, J, et al. Placebo-controlled, randomized trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK Study. Lancet 1989; 1:175.
- ↑ Timothy M. E. Davis, FRACP; Helen Millns, PhD; Irene M. Stratton, MSc; Rury R. Holman, FRCP; Robert C. Turner, MD, FRCP; for the UK Prospective Diabetes Study Group. Risk Factors for Stroke in Type 2 Diabetes Mellitus, United Kingdom Prospective Diabetes Study (UKPDS) 29.Arch Intern Med. 1999;159:1097-1103.
- ↑ PA Wolf, RB D'Agostino, AJ Belanger and WB Kannel Probability of stroke: a risk profile from the Framingham Study. Stroke, Vol 22, 312-318
- ↑ Blauw GJ, Lagaay AM, Smelt AH, Westendorp RG. (1997) Stroke, statins, and cholesterol. A meta-analysis of randomized, placebo-controlled, double-blind trials with HMG-CoA reductase inhibitors. Stroke May;28(5):946-50. PMID 9158630
- ↑ Halliday A, Harrison M, Hayter E, Kong X, Mansfield A, Marro J et al. (2010). "10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (ACST-1): a multicentre randomised trial.". Lancet 376 (9746): 1074-84. DOI:10.1016/S0140-6736(10)61197-X. PMID 20870099. Research Blogging.
- ↑ (November 1996) "A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee". Lancet 348 (9038): 1329–39. PMID 8918275. [e]
- ↑ Diener HC, Bogousslavsky J, Brass LM, et al (2004). "Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial". Lancet 364 (9431): 331–7. DOI:10.1016/S0140-6736(04)16721-4. PMID 15276392. Research Blogging.
- ↑ Verro P, Gorelick PB, Nguyen D (2008). "Aspirin plus dipyridamole versus aspirin for prevention of vascular events after stroke or TIA: a meta-analysis". Stroke 39 (4): 1358-63. DOI:10.1161/STROKEAHA.107.496281. PMID 18323511. Research Blogging.
- ↑ Halkes PH, van Gijn J, Kappelle LJ, Koudstaal PJ, Algra A (May 2006). "Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial". Lancet 367 (9523): 1665–73. DOI:10.1016/S0140-6736(06)68734-5. PMID 16714187. Research Blogging.
- ↑ Sacco RL, Diener HC, Yusuf S, et al (September 2008). "Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke". N. Engl. J. Med. 359 (12): 1238–51. DOI:10.1056/NEJMoa0805002. PMID 18753638. Retrieved on 2008-12-10. Research Blogging.
- ↑ Kent DM, Thaler DE (August 2008). "Stroke Prevention -- Insights from Incoherence". N. Engl. J. Med.. DOI:10.1056/NEJMe0806806. PMID 18753641. Research Blogging.
- ↑ Thijs V, Lemmens R, Fieuws S (May 2008). "Network meta-analysis: simultaneous meta-analysis of common antiplatelet regimens after transient ischaemic attack or stroke". Eur. Heart J. 29 (9): 1086–92. DOI:10.1093/eurheartj/ehn106. PMID 18349026. Research Blogging.
- ↑ Carotid Stenting Trialists' Collaboration. Bonati LH, Dobson J, Algra A, Branchereau A, Chatellier G et al. (2010). "Short-term outcome after stenting versus endarterectomy for symptomatic carotid stenosis: a preplanned meta-analysis of individual patient data.". Lancet 376 (9746): 1062-73. DOI:10.1016/S0140-6736(10)61009-4. PMID 20832852. Research Blogging.
- ↑ Meier P, Knapp G, Tamhane U, Chaturvedi S, Gurm HS (2010). "Short term and intermediate term comparison of endarterectomy versus stenting for carotid artery stenosis: systematic review and meta-analysis of randomised controlled clinical trials.". BMJ 340: c467. DOI:10.1136/bmj.c467. PMID 20154049. Research Blogging.
- ↑ International Carotid Stenting Study investigators. Ederle J, Dobson J, Featherstone RL, Bonati LH, van der Worp HB et al. (2010). "Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (International Carotid Stenting Study): an interim analysis of a randomised controlled trial.". Lancet 375 (9719): 985-97. DOI:10.1016/S0140-6736(10)60239-5. PMID 20189239. Research Blogging.
- ↑ Brott TG, Hobson RW, Howard G, Roubin GS, Clark WM, Brooks W et al. (2010). "Stenting versus endarterectomy for treatment of carotid-artery stenosis.". N Engl J Med 363 (1): 11-23. DOI:10.1056/NEJMoa0912321. PMID 20505173. Research Blogging.