Childbirth: Difference between revisions
imported>Mary Ash No edit summary |
imported>Andrew Steinborn (talk) |
||
| (26 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{subpages}} | ||
{{TOC|right}} | |||
'''Childbirth''', or '''labor and delivery''', is the process by which a woman gives birth to a [[baby]]. Standard Western practice divides the process into three named stages. The first stage of labor involves cervical dilation and has two phases: latent and active. The second stage of labor is the period from the descent of the baby to its actual birth, while the third stage of childbirth is when the placenta is delivered. | |||
Childbirth is often accompanied by severe [[pain]] and attendant anxiety. The woman in labor generally experiences a wide range of complex and intense [[emotion]]s | |||
== Assessment== | |||
Ideally, the person performing the delivery -- a physician or midwife -- has access to prenatal sonograms, laboratory tests, etc. In any event, an experienced operator will palpate the uterus to find the position of the fetus. Vaginal examination will reveal potentially catastrophic complications such as [[placenta previa]]. | |||
Knowledge of [[prenatal care]], or the lack thereof, will alert the delivery team to potential complications of pregnancy and birth. Information from medical care warns of conditions including [[pre-eclampsia]], [[gestational diabetes]], [[herpes]] and [[HIV]] infection, [[hypothyroidism]], [[erythroblastosis fetalis]] and [[tuberculosis]]. | |||
===Station=== | |||
Station is measured by where the baby's head is located in reference to the woman's ischial spines. Measurements above the ischial spines are reported as -1 to -5. Once the baby's head engages into the pelvis, or at 0 station, the baby's placement within the birth canal will be written in positive numbers. The numbers for the positive station are written as +1 to +5. | |||
===Decisions about delivery=== | |||
A variety of factors go into the decision to induce vaginal delivery or to perform caesarian section. | |||
When the [[gestational age]] is less than 36 weeks, the infant is likely to need [[neonatal intensive care]] (NICU), and, unless the baby is crowning or in a very low station, it is better to transfer the mother to a place with an NICU than to deliver the baby and transport it. At least consultation with an obstetrician is wise in the premature birth scenario. <ref>{{citation | |||
| contribution = Chapter 6, Obstetric & Gynecologic Emergencies & Rape | |||
| author = Melissa Platt & Mary Nan Mallory | |||
| editor = C. Keith Stone & Roger L. Humphries | |||
| title = Current Emergency Diagnosis & Treatment | |||
| publisher = Lange/McGraw-Hill | |||
| edition = Fifth Edition | year = 2004 | |||
| isbn = 0838414502 | |||
}}, pp. 746-777</ref> | |||
==Vaginal delivery== | |||
In uncomplicated deliveries, there are a wide range of options about the birth experience. It may be in the home, it may be in a minimally clinical "birthing center", or it may be in a fully equipped labor and delivery suite. | |||
== First | Some mothers prefer "natural childbirth" with no drugs for pain control, routine intravenous lines, or fetal monitoring. Others want more medical support. Pain control is complex, because a number of drugs that make the mother more comfortable also depress the respiration of the baby or the muscular tone needed for delivery. | ||
===First stage of labor=== | |||
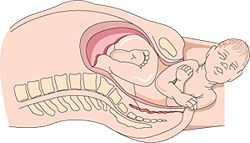
{{Image|Labor-pelvis.jpg|left|250px|Most babies enter the [[birth canal]] facing sideways and the head turns face down.}} | |||
Triggered by the hormone [[oxytocin]], produced in the [[posterior pituitary]], irregular contractions are felt during the latent phase of labor. The contractions will slowly become more regular and pain is minimal. The [[cervix]] will dilate and efface up to 4 [[centimeter]]s during the latent phase of labor. First time mothers will on average labor 8 hours during the latent phase. Mothers who have borne previous children typically have shorter labor during the latent phase. Towards the end of this stage a woman will enter the transition phase. During this part of labor the cervix will continue to dilate to 10 centimeters. This is probably the most painful part of the labor process. | |||
====Cervical dilation==== | |||
Measurement of the cervix is recorded from 0 to 10 centimeters. The cervix is considered complete when it reaches 10 centimeters. | Measurement of the cervix is recorded from 0 to 10 centimeters. The cervix is considered complete when it reaches 10 centimeters. | ||
The cervix shortens in preparation for birth. The normal uneffaced average cervical length is between 3.5 to 4.0 centimeters. | The cervix shortens in preparation for birth. The normal uneffaced average cervical length is between 3.5 to 4.0 centimeters. | ||
====Fetal monitoring==== | |||
====Delaying the first stage==== | |||
If a birth is premature or there are medical reasons to delay vaginal delivery, [[tocolysis|tocolytic drugs]] may be used to suppress uterine contractions. Current agents used to delay premature uterine activity include [[magnesium sulfate]], [[oxytocin]] antagonists, [[calcium channel inhibitor]]s, and [[adrenergic beta-agonist]]s. Ethyl alcohol is obsolete for tocolysis. | |||
===Second stage of labor=== | |||
The cervix is fully dilated and the woman begins to push to deliver the baby. This phase of labor can last many hours, although the condition of the mother and baby, not an arbitrary time, determines if surgical intervention is needed. <ref>{{citation | |||
| title = Is there an upper time limit for the management of the second stage of labor? | |||
| author = Aaron B. Caughey | |||
| journal = American Journal of Obstetrics & Gynecology | |||
| date = October 2009| volume = 201| issue = 4 | pages = 337-338 | |||
| url = http://www.ajog.org/article/S0002-9378%2809%2900902-8/fulltext | |||
}}</ref> | |||
In non-Western cultures, the baby is often delivered in a different position than the supine, feet-in-stirrups used in Western delivery rooms. A Cochrane review suggesed that kneeling or standing may be more comfortable for a mother, as long as epidural anesthesia is not used. The risk of bleeding, however may be lessened in the supine position. <ref>{{citation | |||
|author = Gupta JK, Hofmeyr GJ, Smyth RMD | |||
| title = Position in the second stage of labour for women without epidural anaesthesia | |||
| journal = Cochrane Database of Systematic Reviews | year = 2000 | Issue=1 |doi=10.1002/14651858.CD002006.pub2 | |||
| url = http://www2.cochrane.org/reviews/en/ab002006.html}}</ref> | |||
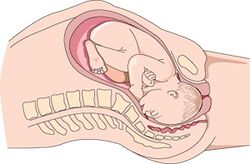
The baby is delivered at the end of the second stage of labor. The [[umbilical cord]] is cut by the doctor once the delivery is finished.{{Image|Labor-head.jpg|right|250px|The head emerging from the birth canal.}} | |||
====Comfort measures==== | |||
The experience of pain varies with the emotional of the mother as well as the physical realities. It is an intensely emotional experience, and emotions have much to do with pain tolerance. Nonpharmacologic measures are always preferable for controlling discomfort, such as encouragement from one (or sometimes more) people there purely to support the mother, such as the father or a labor assistant called a ''[[doula]]''. | |||
== Cesarean | [[Epidural anesthesia]] is one means of controlling pain, which also has minimal effect on the baby's respiration. It usually requires a second medical professional to administer. | ||
====Episiotomy==== | |||
A small incision, or cut, used to enlarge the vaginal opening. The person performing the delivery sutures the area once the delivery is finished. This is not always done during a vaginal delivery, and, indeed, is quite controversial.<ref>{{citation | |||
| title = New ACOG Opinion Addresses Elective Cesarean Controversy | |||
| url = http://www.acog.org/from_home/publications/press_releases/nr10-31-03-1.cfm | |||
| publisher = [[American College of Obstetrics and Gynecology]] | |||
| date = 31 October 2003}}</ref> One of the risks is inducing perineal and anorectal damage. <ref>{{citation | |||
| author = Kudish B, Blackwell S, McNeeley SG ''et al.'' | |||
| title = Operative vaginal delivery and midline episiotomy: a bad combination for the perineum | |||
| journal = Am. J. Obstet. Gynecol | volume = 195 | pages = 749–754 | year = 2006}}</ref> In a study of 258 episiotomies," of whom 98 (41%) had mediolateral episiotomies. Of these, 58 were delivered by physicians and 40 by midwives. The investigators found that episiotomies cut by doctors were longer and deeper than those cut by midwives. Only 22% of episiotomies cut by doctors were truly mediolateral (between 40 and 60°), and none of the episiotomies cut by midwives met these criteria." The angle of the episiotomy may be a risk factor for anal damage. <ref>{{citation | |||
| author = Eogan M, Daly L, O'Connell PR, O'Herlihy C | |||
| title = Does the angle of episiotomy affect the incidence of anal sphincter injury? | |||
| journal = Br. J. Obstet. Gynaecol | volume = 113 | issue = 2 | pages = 190–194 | year =2006 | |||
}}</ref> | |||
===Third stage of labor=== | |||
The [[placenta]] is delivered during the third stage of labor. Usually this phase of labor takes between 5 to 20 minutes. | |||
== Cesarean section == | |||
The cesarean is when a baby is surgically removed from the uterus. Most cesarean section usually takes up to an hour to complete. The surgeon normally makes two cuts in the lower abdomen before making an incision in the uterus. The baby is removed from the uterus and the umbilical cord is cut. | The cesarean is when a baby is surgically removed from the uterus. Most cesarean section usually takes up to an hour to complete. The surgeon normally makes two cuts in the lower abdomen before making an incision in the uterus. The baby is removed from the uterus and the umbilical cord is cut. | ||
==References== | |||
{{reflist|2}} | |||
Latest revision as of 16:18, 4 August 2010
Childbirth, or labor and delivery, is the process by which a woman gives birth to a baby. Standard Western practice divides the process into three named stages. The first stage of labor involves cervical dilation and has two phases: latent and active. The second stage of labor is the period from the descent of the baby to its actual birth, while the third stage of childbirth is when the placenta is delivered.
Childbirth is often accompanied by severe pain and attendant anxiety. The woman in labor generally experiences a wide range of complex and intense emotions
Assessment
Ideally, the person performing the delivery -- a physician or midwife -- has access to prenatal sonograms, laboratory tests, etc. In any event, an experienced operator will palpate the uterus to find the position of the fetus. Vaginal examination will reveal potentially catastrophic complications such as placenta previa.
Knowledge of prenatal care, or the lack thereof, will alert the delivery team to potential complications of pregnancy and birth. Information from medical care warns of conditions including pre-eclampsia, gestational diabetes, herpes and HIV infection, hypothyroidism, erythroblastosis fetalis and tuberculosis.
Station
Station is measured by where the baby's head is located in reference to the woman's ischial spines. Measurements above the ischial spines are reported as -1 to -5. Once the baby's head engages into the pelvis, or at 0 station, the baby's placement within the birth canal will be written in positive numbers. The numbers for the positive station are written as +1 to +5.
Decisions about delivery
A variety of factors go into the decision to induce vaginal delivery or to perform caesarian section.
When the gestational age is less than 36 weeks, the infant is likely to need neonatal intensive care (NICU), and, unless the baby is crowning or in a very low station, it is better to transfer the mother to a place with an NICU than to deliver the baby and transport it. At least consultation with an obstetrician is wise in the premature birth scenario. [1]
Vaginal delivery
In uncomplicated deliveries, there are a wide range of options about the birth experience. It may be in the home, it may be in a minimally clinical "birthing center", or it may be in a fully equipped labor and delivery suite.
Some mothers prefer "natural childbirth" with no drugs for pain control, routine intravenous lines, or fetal monitoring. Others want more medical support. Pain control is complex, because a number of drugs that make the mother more comfortable also depress the respiration of the baby or the muscular tone needed for delivery.
First stage of labor
Most babies enter the birth canal facing sideways and the head turns face down.
Triggered by the hormone oxytocin, produced in the posterior pituitary, irregular contractions are felt during the latent phase of labor. The contractions will slowly become more regular and pain is minimal. The cervix will dilate and efface up to 4 centimeters during the latent phase of labor. First time mothers will on average labor 8 hours during the latent phase. Mothers who have borne previous children typically have shorter labor during the latent phase. Towards the end of this stage a woman will enter the transition phase. During this part of labor the cervix will continue to dilate to 10 centimeters. This is probably the most painful part of the labor process.
Cervical dilation
Measurement of the cervix is recorded from 0 to 10 centimeters. The cervix is considered complete when it reaches 10 centimeters.
The cervix shortens in preparation for birth. The normal uneffaced average cervical length is between 3.5 to 4.0 centimeters.
Fetal monitoring
Delaying the first stage
If a birth is premature or there are medical reasons to delay vaginal delivery, tocolytic drugs may be used to suppress uterine contractions. Current agents used to delay premature uterine activity include magnesium sulfate, oxytocin antagonists, calcium channel inhibitors, and adrenergic beta-agonists. Ethyl alcohol is obsolete for tocolysis.
Second stage of labor
The cervix is fully dilated and the woman begins to push to deliver the baby. This phase of labor can last many hours, although the condition of the mother and baby, not an arbitrary time, determines if surgical intervention is needed. [2]
In non-Western cultures, the baby is often delivered in a different position than the supine, feet-in-stirrups used in Western delivery rooms. A Cochrane review suggesed that kneeling or standing may be more comfortable for a mother, as long as epidural anesthesia is not used. The risk of bleeding, however may be lessened in the supine position. [3]
The baby is delivered at the end of the second stage of labor. The umbilical cord is cut by the doctor once the delivery is finished.
Comfort measures
The experience of pain varies with the emotional of the mother as well as the physical realities. It is an intensely emotional experience, and emotions have much to do with pain tolerance. Nonpharmacologic measures are always preferable for controlling discomfort, such as encouragement from one (or sometimes more) people there purely to support the mother, such as the father or a labor assistant called a doula.
Epidural anesthesia is one means of controlling pain, which also has minimal effect on the baby's respiration. It usually requires a second medical professional to administer.
Episiotomy
A small incision, or cut, used to enlarge the vaginal opening. The person performing the delivery sutures the area once the delivery is finished. This is not always done during a vaginal delivery, and, indeed, is quite controversial.[4] One of the risks is inducing perineal and anorectal damage. [5] In a study of 258 episiotomies," of whom 98 (41%) had mediolateral episiotomies. Of these, 58 were delivered by physicians and 40 by midwives. The investigators found that episiotomies cut by doctors were longer and deeper than those cut by midwives. Only 22% of episiotomies cut by doctors were truly mediolateral (between 40 and 60°), and none of the episiotomies cut by midwives met these criteria." The angle of the episiotomy may be a risk factor for anal damage. [6]
Third stage of labor
The placenta is delivered during the third stage of labor. Usually this phase of labor takes between 5 to 20 minutes.
Cesarean section
The cesarean is when a baby is surgically removed from the uterus. Most cesarean section usually takes up to an hour to complete. The surgeon normally makes two cuts in the lower abdomen before making an incision in the uterus. The baby is removed from the uterus and the umbilical cord is cut.
References
- ↑ Melissa Platt & Mary Nan Mallory (2004), Chapter 6, Obstetric & Gynecologic Emergencies & Rape, in C. Keith Stone & Roger L. Humphries, Current Emergency Diagnosis & Treatment (Fifth Edition ed.), Lange/McGraw-Hill, ISBN 0838414502, pp. 746-777
- ↑ Aaron B. Caughey (October 2009), "Is there an upper time limit for the management of the second stage of labor?", American Journal of Obstetrics & Gynecology 201 (4): 337-338
- ↑ Gupta JK, Hofmeyr GJ, Smyth RMD (2000), "Position in the second stage of labour for women without epidural anaesthesia", Cochrane Database of Systematic Reviews, DOI:10.1002/14651858.CD002006.pub2
- ↑ New ACOG Opinion Addresses Elective Cesarean Controversy, American College of Obstetrics and Gynecology, 31 October 2003
- ↑ Kudish B, Blackwell S, McNeeley SG et al. (2006), "Operative vaginal delivery and midline episiotomy: a bad combination for the perineum", Am. J. Obstet. Gynecol 195: 749–754
- ↑ Eogan M, Daly L, O'Connell PR, O'Herlihy C (2006), "Does the angle of episiotomy affect the incidence of anal sphincter injury?", Br. J. Obstet. Gynaecol 113 (2): 190–194