Adrenergic beta-antagonist: Difference between revisions
imported>Robert Badgett |
imported>Robert Badgett |
||
| Line 119: | Line 119: | ||
Beta-blockers may not be a good first choice medication in treating hypertension - at least for patients without [[coronary heart disease]].<ref name="pmid16257341">{{cite journal |author=Lindholm LH, Carlberg B, Samuelsson O |title=Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis |journal=Lancet |volume=366 |issue=9496 |pages=1545–53 |year=2005 |pmid=16257341 |doi=10.1016/S0140-6736(05)67573-3 |url=http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(05)67573-3 |issn=}}</ref> A [[meta-analysis]] has concluded that the more the drug lowers the [[heart rate]], the lower the benefit of the drug.<ref name="pmid19017516">{{cite journal |author=Bangalore S, Sawhney S, Messerli FH |title=Relation of beta-blocker-induced heart rate lowering and cardioprotection in hypertension |journal=J. Am. Coll. Cardiol. |volume=52 |issue=18 |pages=1482–9 |year=2008 |month=October |pmid=19017516 |doi=10.1016/j.jacc.2008.06.048 |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(08)02724-1 |issn=}}</ref><ref name="pmid19017517">{{cite journal |author=Kaplan NM |title=Beta-blockers in hypertension: adding insult to injury |journal=J. Am. Coll. Cardiol. |volume=52 |issue=18 |pages=1490–1 |year=2008 |month=October |pmid=19017517 |doi=10.1016/j.jacc.2008.08.008 |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(08)02719-8 |issn=}}</ref> Alternatively, or in addition: | Beta-blockers may not be a good first choice medication in treating hypertension - at least for patients without [[coronary heart disease]].<ref name="pmid16257341">{{cite journal |author=Lindholm LH, Carlberg B, Samuelsson O |title=Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis |journal=Lancet |volume=366 |issue=9496 |pages=1545–53 |year=2005 |pmid=16257341 |doi=10.1016/S0140-6736(05)67573-3 |url=http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(05)67573-3 |issn=}}</ref> A [[meta-analysis]] has concluded that the more the drug lowers the [[heart rate]], the lower the benefit of the drug.<ref name="pmid19017516">{{cite journal |author=Bangalore S, Sawhney S, Messerli FH |title=Relation of beta-blocker-induced heart rate lowering and cardioprotection in hypertension |journal=J. Am. Coll. Cardiol. |volume=52 |issue=18 |pages=1482–9 |year=2008 |month=October |pmid=19017516 |doi=10.1016/j.jacc.2008.06.048 |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(08)02724-1 |issn=}}</ref><ref name="pmid19017517">{{cite journal |author=Kaplan NM |title=Beta-blockers in hypertension: adding insult to injury |journal=J. Am. Coll. Cardiol. |volume=52 |issue=18 |pages=1490–1 |year=2008 |month=October |pmid=19017517 |doi=10.1016/j.jacc.2008.08.008 |url=http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(08)02719-8 |issn=}}</ref> Alternatively, or in addition: | ||
* beta-blockers may not lower the central aortic pressure as much other anti-hypertensive agents despite similar effects on the brachial systolic pressure.<ref name="pmid16476843">{{cite journal |author=Williams B, Lacy PS, Thom SM, ''et al.'' |title=Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study |journal=Circulation |volume=113 |issue=9 |pages=1213–25 |year=2006 |month=March |pmid=16476843 |doi=10.1161/CIRCULATIONAHA.105.595496 |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=16476843 |issn=}}</ref> | * beta-blockers may not lower the central aortic pressure as much other anti-hypertensive agents despite similar effects on the brachial systolic pressure.<ref name="pmid16476843">{{cite journal |author=Williams B, Lacy PS, Thom SM, ''et al.'' |title=Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study |journal=Circulation |volume=113 |issue=9 |pages=1213–25 |year=2006 |month=March |pmid=16476843 |doi=10.1161/CIRCULATIONAHA.105.595496 |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=16476843 |issn=}}</ref> | ||
* beta-blocker trials suffer from not doing beta-blockers often enough. | * beta-blocker trials suffer from not doing beta-blockers often enough. Most trials in the meta-analysis used atenolol once per day. Only in the INVEST trial, atenolol was dosed twice a day if needed and in this trial atenolol was as effective as a calcium channel blocker.<ref name="pmid14657064">{{cite journal |author=Pepine CJ, Handberg EM, Cooper-DeHoff RM, ''et al.'' |title=A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial |journal=JAMA |volume=290 |issue=21 |pages=2805–16 |year=2003 |month=December |pmid=14657064 |doi=10.1001/jama.290.21.2805 |url=http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=14657064 |issn=}}</ref> | ||
Beta-blockers may be less effective than [[diuretic]]s in the treatment of elderly patients with [[hypertension]] due to reduced ability to prevent [[coronary heart disease]].<ref name="pmid9634263">{{cite journal |author=Messerli FH, Grossman E, Goldbourt U |title=Are beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic review |journal=JAMA |volume=279 |issue=23 |pages=1903–7 |year=1998 |month=June |pmid=9634263 |doi= |url=http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=9634263 |issn=}}</ref> | Beta-blockers may be less effective than [[diuretic]]s in the treatment of elderly patients with [[hypertension]] due to reduced ability to prevent [[coronary heart disease]].<ref name="pmid9634263">{{cite journal |author=Messerli FH, Grossman E, Goldbourt U |title=Are beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic review |journal=JAMA |volume=279 |issue=23 |pages=1903–7 |year=1998 |month=June |pmid=9634263 |doi= |url=http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=9634263 |issn=}}</ref> | ||
Revision as of 04:32, 31 July 2009
Adrenergic beta-receptor blockaders (beta-blockers) are "drugs that bind to but do not activate beta-adrenergic receptors thereby blocking the actions of beta-adrenergic agonists. Adrenergic beta-antagonists are used for treatment of hypertension, cardiac arrhythmias, angina pectoris, glaucoma, migraine headaches, and anxiety".[1]
Beta-blockers vary within the class regarding their properties. Beta-blockers that have low intrinsic sympathomimetic activity (ISA), low membrane stabilizing activity, high beta 1-selectivity, and high lipophilicity may be more effective.[2]
Classification
Generically available beta-blockers, which subclassify based on selective aspects of their action, include: include:[3][4]
- Acebutolol
- Atenolol
- Bisoprolol
- Metoprolol
- Nadolol
- Propranolol
- Timolol
They further divide by frequency of dosing, cost, and other factors.
| Selectivity | Agents | Applications |
|---|---|---|
| Nonselective | propranolol, timolol, nadolol, pindolol, penbutolol, carteolol | migraine (propranolol) |
| Cardioselective/beta 1-selectivity | Atenolol, Metoprolol, Bisoprolol, Metoprolol, Acebutolol, Betaxolol | myocardial infarction (metoprolol), heart failure (Carvedilol) |
| Intrinsic sympathomimetic activity | Acebutolol, Pindolol, Penbutolol | row 2, cell 3 |
| Beta-blockers with alpha blocking activity | Carvedilol, Labetalol | Heart failure (Carvedilol) |
Cardioselective/beta 1-selectivity
Generic beta-blockers with beta 1-selectivity:[3][5]
- Atenolol
- Bisoprolol
- Metoprolol
- Hepatically metabolized by cytochrome P-450 2D6 allele
- Lipophilic[6]
- Acebutolol
Non-generic:
- Betaxolol
Non-selective
Non-selective drugs include propranolol, timolol, nadolol, pindolol, penbutolol, and carteolol.
Intrinsic sympathomimetic activity
Generic beta-blockers with intrinsic sympathomimetic activity (less resting bradycardia and lipid changes):[3]
- Acebutolol
- Pindolol
Non-generic:
- Penbutolol
Beta-blockers with alpha blocking activity
Generic beta-blockers with alpha blocking activity (more orthostatic hypotension):[3]
- Carvedilol
- Labetalol
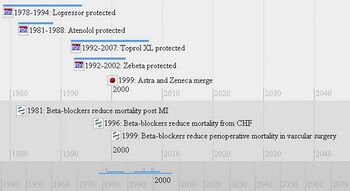
History
Propranolol was developed by James Black who later received the Nobel Prize for this and other work.[8]
Pharmacogenetics
The pharmacogenetics of beta-blockers have been reviewed.[9]
G-protein-coupled receptor kinase
Regarding the treatment of heart failure, there is conflicting evidence whether beta-blockers are as effective in African-American patients as in Anglo patients.[10] This may be due to a polymorphism in African-American patients of the G-protein-coupled receptor kinase (GRK5) (OMIM) that confers a natural "genetic beta-blockade".[11]
Adrenergic receptor
Variation adrenergic receptor genotype may also influence effectiveness.[12]
Cytochrome P-450
Beta-blockers such as metoprolol that are metabolized by cytochrome P-450 2D6 allele and may have more drug interactions[13] and inherited variations in metabolism.[14]
Although poor metabolism due to CYP2D6 polymorphisms may be present in patients with drug toxicity due to metoprolol[15], small studies suggest that careful, slow titration [16][17] and avoidance of other drugs metabolized by CYP2D6[18] may avoid drug toxicity from polymorphisms of cytochrome P-450.
Dosage
In the 1980s, beta-blockers were thought to be effective if given once daily.[19][20][21] However, in the 1990s recognition occurred that beta-blockers varied on their duration of action.[22]
Clinical uses
The effect of adrenergic beta-antagonists on heart rate may be more predictive than the amount of drug in predicting the drug's benefit[23] or harm[24]. This may be due to invidual molecular variations in adrenergic receptors, G-protein-coupled receptor kinases, and metabolism by cytochrome P-450.
The individual beta-blockers have been compared in the treatment of various diseases.[25]
Coronary heart disease
Adrenergic beta-antagonists were first shown to be effective in 1981.[26]
Meta-analyses have concluded that metoprolol may[2] or may not[27] be the best beta-blocker for secondary prevention of myocardial infarctions.
Heart failure
Beta-blockers were originally thought to be contraindicated in patients with heart failure. However, trials eventually showed benefit of the drugs.Metoprolol can benefit patients with heart failure.[28][29]
Two cohort studies suggest that atenolol and carvedilol may be more effect than metoprolol for the treatment of heart failure.[30][31]
Drugs with intrinsic sympathomimetic activity may have less benefit[27] A systematic review of randomized controlled trials concluded "metoprolol, carvedilol, and bisoprolol all exhibited statistically significant mortality rate reductions compared with placebo, the data were inconclusive for nebivolol or atenolol" and "for every heart rate reduction of 5 beats/min with β-blocker treatment, a commensurate 18% reduction in the risk for death occurred."[23]
Hypertension
Beta-blockers may not be a good first choice medication in treating hypertension - at least for patients without coronary heart disease.[32] A meta-analysis has concluded that the more the drug lowers the heart rate, the lower the benefit of the drug.[24][33] Alternatively, or in addition:
- beta-blockers may not lower the central aortic pressure as much other anti-hypertensive agents despite similar effects on the brachial systolic pressure.[34]
- beta-blocker trials suffer from not doing beta-blockers often enough. Most trials in the meta-analysis used atenolol once per day. Only in the INVEST trial, atenolol was dosed twice a day if needed and in this trial atenolol was as effective as a calcium channel blocker.[35]
Beta-blockers may be less effective than diuretics in the treatment of elderly patients with hypertension due to reduced ability to prevent coronary heart disease.[36]
References
- ↑ Anonymous (2024), Adrenergic beta-antagonist (English). Medical Subject Headings. U.S. National Library of Medicine.
- ↑ 2.0 2.1 Soriano JB, Hoes AW, Meems L, Grobbee DE (1997). "Increased survival with beta-blockers: importance of ancillary properties". Prog Cardiovasc Dis 39 (5): 445–56. PMID 9122425. [e]
- ↑ 3.0 3.1 3.2 3.3 (June 2005) "Drugs for hypertension". Treat Guidel Med Lett 3 (34): 39–48. PMID 15912125. [e]
- ↑ (March 2008) "Nebivolol (Bystolic) for hypertension". Med Lett Drugs Ther 50 (1281): 17–9. PMID 18323772. [e]
- ↑ (January 2009) "Drugs for hypertension". Treat Guidel Med Lett 7 (77): 1–10. PMID 19107095. [e]
- ↑ 6.0 6.1 Tuininga YS, Crijns HJ, Brouwer J, et al (December 1995). "Evaluation of importance of central effects of atenolol and metoprolol measured by heart rate variability during mental performance tasks, physical exercise, and daily life in stable postinfarct patients". Circulation 92 (12): 3415–23. PMID 8521562. [e]
- ↑ Sarafidis P, Bogojevic Z, Basta E, Kirstner E, Bakris GL (February 2008). "Comparative efficacy of two different beta-blockers on 24-hour blood pressure control". J Clin Hypertens (Greenwich) 10 (2): 112–8. PMID 18259123. [e]
- ↑ Stapleton MP (1997). "Sir James Black and propranolol. The role of the basic sciences in the history of cardiovascular pharmacology". Tex Heart Inst J 24 (4): 336–42. PMID 9456487. PMC 325477. [e]
- ↑ Shin J, Johnson JA (June 2007). "Pharmacogenetics of beta-blockers". Pharmacotherapy 27 (6): 874–87. DOI:10.1592/phco.27.6.874. PMID 17542770. Research Blogging.
- ↑ Shekelle PG, Rich MW, Morton SC, et al (2003). "Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: a meta-analysis of major clinical trials". J. Am. Coll. Cardiol. 41 (9): 1529–38. PMID 12742294. [e]
- ↑ Liggett, Stephen B et al. 2008. A GRK5 polymorphism that inhibits [beta]-adrenergic receptor signaling is protective in heart failure. Nat Med advanced online publication. http://dx.doi.org/10.1038/nm1750 (Accessed April 29, 2008).
- ↑ Zaugg M, Bestmann L, Wacker J, et al (July 2007). "Adrenergic receptor genotype but not perioperative bisoprolol therapy may determine cardiovascular outcome in at-risk patients undergoing surgery with spinal block: the Swiss Beta Blocker in Spinal Anesthesia (BBSA) study: a double-blinded, placebo-controlled, multicenter trial with 1-year follow-up". Anesthesiology 107 (1): 33–44. DOI:10.1097/01.anes.0000267530.62344.a4. PMID 17585213. Research Blogging.
- ↑ Onalan O, Cumurcu BE, Bekar L (May 2008). "Complete atrioventricular block associated with concomitant use of metoprolol and paroxetine". Mayo Clin. Proc. 83 (5): 595–9. PMID 18452693. [e]
- ↑ Nozawa T, Taguchi M, Tahara K, et al (November 2005). "Influence of CYP2D6 genotype on metoprolol plasma concentration and beta-adrenergic inhibition during long-term treatment: a comparison with bisoprolol". J. Cardiovasc. Pharmacol. 46 (5): 713–20. PMID 16220080. [e]
- ↑ Wuttke H, Rau T, Heide R, et al. (October 2002). "Increased frequency of cytochrome P450 2D6 poor metabolizers among patients with metoprolol-associated adverse effects". Clin. Pharmacol. Ther. 72 (4): 429–37. DOI:10.1067/mcp.2002.127111. PMID 12386645. Research Blogging.
- ↑ Terra SG, Pauly DF, Lee CR, et al. (March 2005). "beta-Adrenergic receptor polymorphisms and responses during titration of metoprolol controlled release/extended release in heart failure". Clin. Pharmacol. Ther. 77 (3): 127–37. DOI:10.1016/j.clpt.2004.10.006. PMID 15735607. Research Blogging.
- ↑ Zineh I, Beitelshees AL, Gaedigk A, et al. (December 2004). "Pharmacokinetics and CYP2D6 genotypes do not predict metoprolol adverse events or efficacy in hypertension". Clin. Pharmacol. Ther. 76 (6): 536–44. DOI:10.1016/j.clpt.2004.08.020. PMID 15592325. Research Blogging.
- ↑ Fux R, Mörike K, Pröhmer AM, et al. (October 2005). "Impact of CYP2D6 genotype on adverse effects during treatment with metoprolol: a prospective clinical study". Clin. Pharmacol. Ther. 78 (4): 378–87. DOI:10.1016/j.clpt.2005.07.004. PMID 16198657. Research Blogging.
- ↑ Kaplan, Norman M.; Lieberman, Ellin (1990). “Treatment of Hypertension: Drug Therapy”, Clinical Hypertension, Fifth. Baltimore: Williams & Wilkins, 220. ISBN 0-683-04522-9. “All beta-blockers act longer on the blood pressure than the pharmacokinetic data would imply. In moderate doses, most beta-blokders will likely keep the blood pressure down when given once daily. To ensure adequate control, early morning blodd presures should be measured before the daily dose is taken”
- ↑ Johansson SR, McCall M, Wilhelmsson C, Vedin JA (May 1980). "Duration of action of beta blockers". Clin. Pharmacol. Ther. 27 (5): 593–601. PMID 6102896. [e]
- ↑ Watson RD, Stallard TJ, Littler WA (June 1979). "Influence of once-daily administration of beta-adrenoceptor antagonists on arterial pressure and its variability". Lancet 1 (8128): 1210–3. PMID 87678. “Patients were treated with either propranolol 240 mg (8 patients), metoprolol 200 mg (8 patients), or acebutolol 400 mg (4 patients) taken once daily.” [e]
- ↑ Kaplan, Norman M.; Lieberman, Ellin (1994). “Treatment of Hypertension: Drug Therapy”, Clinical Hypertension, Sixth. Baltimore: Williams & Wilkins, 225. ISBN 0-683-04544-X. “In the usual doses prescribed, various beta blockers have equal antihypertensive efficacy. However, they many not all provide full 24-hour lowering of the BP which may be particularly critical in protecting against early morning cardiovascular catastrophes. Metoprolol blunted this rise, but atenolol and pindolol did not (Raferty and Carrageta, 1985). Neutel et al, (1990) found a similar lack of 24-hour effect with once-daily atenolol but a sustained effect with acebutolol. Moreover, twice-daily doses of "cardioselective" agents may preserve this cardioselectivity better than once-daily large doses (Lipworth et al, 1991).”
- ↑ 23.0 23.1 McAlister FA, Wiebe N, Ezekowitz JA, Leung AA, Armstrong PW (June 2009). "Meta-analysis: beta-blocker dose, heart rate reduction, and death in patients with heart failure". Ann. Intern. Med. 150 (11): 784–94. PMID 19487713. [e]
- ↑ 24.0 24.1 Bangalore S, Sawhney S, Messerli FH (October 2008). "Relation of beta-blocker-induced heart rate lowering and cardioprotection in hypertension". J. Am. Coll. Cardiol. 52 (18): 1482–9. DOI:10.1016/j.jacc.2008.06.048. PMID 19017516. Research Blogging.
- ↑ Dean L (2007). “Comparing Beta Blockers”, PubMed Clinical Q&A. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information. “Based on Oregon Drug Effectiveness Review Project”
- ↑ (April 1981) "Timolol-induced reduction in mortality and reinfarction in patients surviving acute myocardial infarction". N. Engl. J. Med. 304 (14): 801–7. PMID 7010157. [e]
- ↑ 27.0 27.1 Freemantle N, Cleland J, Young P, Mason J, Harrison J (June 1999). "beta Blockade after myocardial infarction: systematic review and meta regression analysis". BMJ 318 (7200): 1730–7. PMID 10381708. PMC 31101. [e]
- ↑ Waagstein F, Bristow MR, Swedberg K, et al (December 1993). "Beneficial effects of metoprolol in idiopathic dilated cardiomyopathy. Metoprolol in Dilated Cardiomyopathy (MDC) Trial Study Group". Lancet 342 (8885): 1441–6. PMID 7902479. [e]
- ↑ Packer M, Bristow MR, Cohn JN, et al (May 1996). "The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group". N. Engl. J. Med. 334 (21): 1349–55. PMID 8614419. [e]
- ↑ Kramer JM, Curtis LH, Dupree CS, et al (December 2008). "Comparative effectiveness of beta-blockers in elderly patients with heart failure". Arch. Intern. Med. 168 (22): 2422–8; discussion 2428–32. DOI:10.1001/archinternmed.2008.511. PMID 19064824. Research Blogging.
- ↑ Go AS, Yang J, Gurwitz JH, Hsu J, Lane K, Platt R (December 2008). "Comparative effectiveness of different beta-adrenergic antagonists on mortality among adults with heart failure in clinical practice". Arch. Intern. Med. 168 (22): 2415–21. DOI:10.1001/archinternmed.2008.506. PMID 19064823. Research Blogging.
- ↑ Lindholm LH, Carlberg B, Samuelsson O (2005). "Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis". Lancet 366 (9496): 1545–53. DOI:10.1016/S0140-6736(05)67573-3. PMID 16257341. Research Blogging.
- ↑ Kaplan NM (October 2008). "Beta-blockers in hypertension: adding insult to injury". J. Am. Coll. Cardiol. 52 (18): 1490–1. DOI:10.1016/j.jacc.2008.08.008. PMID 19017517. Research Blogging.
- ↑ Williams B, Lacy PS, Thom SM, et al. (March 2006). "Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study". Circulation 113 (9): 1213–25. DOI:10.1161/CIRCULATIONAHA.105.595496. PMID 16476843. Research Blogging.
- ↑ Pepine CJ, Handberg EM, Cooper-DeHoff RM, et al. (December 2003). "A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial". JAMA 290 (21): 2805–16. DOI:10.1001/jama.290.21.2805. PMID 14657064. Research Blogging.
- ↑ Messerli FH, Grossman E, Goldbourt U (June 1998). "Are beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic review". JAMA 279 (23): 1903–7. PMID 9634263. [e]