Herpes
Herpes refers to the diseases caused by Herpes Simplex Virus (HSV). In humans, symptomatic herpes simplex infections take two common forms, a recurrent rash of swollen blisters in the area of the mouth, and a similar rash in the area of the genitals. The two subtypes are responsible for cold sores and genital herpes, a recurrent, painful genital rash. Genital herpes is considered a sexually transmitted disease (STD).
There are other species of Herpes virus that are also human pathogens, notably Herpes Zoster, the cause of both chicken pox (in acute infection) and shingles (chronic infection with reactivation). However, most commonly, the word "herpes" refers to conditions caused by Herpes simplex.
The virus
Herpes Simplex Virus (HSV) is a member of the Herpesviridae family of viruses, a family of DNA viruses important in human disease. These include Human herpesviruses (HHV)1-8 (see Herpes Viruses). HSV 1 and 2 correspond to HHV 1 and 2, and both are very prevalent in the human population, with as many as 30-70% of all people testing positive for antibodies in their lifetime.
Natural history of human infection
HSV 1 and 2 are DNA viruses that cause common human illnesses. In both types, once infection is established it is life-long. These viruses generally cause mucocutaneous infection. This can manifest as cold sores on the lips, or as genital sores. The typical rash has been described as "dew drops on a rose petal", it consists of vesicles (blisters) that are initially clear and then crust over, typically with yellowish exudate. These vesicles are generally painful, and further, the area of skin and/or mucosa and the subcutaneous tissues in the region where the rash will appear commonly becomes sensitive and even swollen before eruption of the vesicles. Tissue swellinfg may increase as the rash blossoms, and then, generaly over a course of a week to 2 weeks, resolves completely - leaving no scarring.
The initial infection with the virus is called the primary infection, and can be accompanied by systemic systems such as fever and muscle aches. After resolution of the symptoms of the primary infection, the virus becomes dormant in the human host. Under certain conditions that are not well understood, the virus is reactivated, with a recurrence of mucocutaneous lesions. These recurrent attacks are unpredictable and can be frequent or infrequent. However, decreased host resistance is often correlated with recurrent attacks. The name "cold sore" for the typical Herpes simplex 1 lesion on the lip comes about because the sores will appear with the onset of an unrelated upper respiratory virus, and these lesions also recur in times of stress and other illnesses. However, recurrences can occur even when the infected person feels well and is under no apparent stress.
In general, lesions from HSV 1 are more commonly seen on the face, but also accounts for a large minority of genital infections. HSV 2 lesions are much more commonly seen on the genitalia than the face. Although genital lesions are a form of STD, other lesions can be contracted without sexual contact. Regardless of how they were contracted, however, an infected person can spread virus to another person with mucosa to mucosa or skin to mucosa contact.
Transmission can occur when sores are visible, as well as when there are no visible lesions. In addition to the common mucocutaneous infection, HSV 1 and 2 can also cause keratitis (inflammation in the eye), encephalitis (brain infection), and severe neonatal disease if acquired during pregnancy.
Diagnosis
The diagnosis of a herpes simplex infection is ordinarily a clinical one, that is- it is made by a trained health care provider based on the patient's history and physical findings, rather than on laboratory tests. However, a clinical diagnosis does not distinguish between HSV-1 and HSV-2 infection, except by probability. Confirming a diagnosis and clarifying the actual virus type involve requires laboratory testing. The most definitive proof of infection, the "gold standard" of diagnostic test, is the growth of the virus in artificial culture from a specimen taken from the patient's lesions. Although primary ulcers have a high rate of viral shed, recurrent lesions shed virus at a much lower rate, and so culture of recurrent lesions has a high false negative rate. Accordingly, in patients with typical presentations of recurrent outbreaks known to be caused by the Herpes Simplex virus, failure to culture the virus in no way overturns the diagnosis.
Viral culture is an expensive laboratory test that must be carried out for 10 days in order to assume negative results.
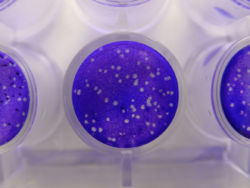
"PCR techniques are more sensitive than viral cuture and results can be available in less than 4 hours". [1]
Diagnostic tests on the immune response to the virus can determine not only the subtype of herpes simplex infection but whether the outbreak is primary or recurrent. HSV-1 and HSV-2 each have respective variations in virally produced glycoprotein G, and immunoglobulin G (IgG) produced by an infected person differs accordingly. If an individual is making IgG to either type of virus, 1 or 2, infection is confirmed. If the individual has cear signs of a genital herpes infection, but the tests for IGG are negative, the most likely explanation is that this is a primary outbreak, and the patient has not yet begun production of that type of antibody. Confirmation of that presumed diagnosis of a primary herpes infection can be made on follow-up testing, with demonstration of anti-HSV IgG levels.
Oral herpes infection
Genital herpes infection
In population studies in the United States, both serotypes of the herpes virus are prevalent in symptomatic genital herpes infections. HSV-2 accounting for more than half, and HSV-1 for almost half, of all nfections. More than 50 million people are infected in that country, making this the most common STD in the USA.
Although both types of herpes simplex virus can account for genital herpes, and cause a very similar appearing rash, "HSV-1 has a much lower recurrence rate. For example, 40% of patients with an initial episode of HSV-1 will remain asymptomatic during the first year of infection, while 40% of patients with an initial outbreak of HSV-2 will have six or more recurrences per year." [2]
The Center for Disease Control (CDC) in the United States recommends that genital lesions be cultured in order to determine the type of HSV infection.
Ophthalmologic herpes simplex infection (eye)
"Herpetic eye disease is among the most common causes for infectious uveitis. It may affect healthy as well as immune-compromised hosts, although its clinical presentation varies accordingly."
Herpes encephalitis
Herpes simplex infection in neonates
Although herpes infection is aggravating in healthy adults, it is a lethal disease in very young babies.
"Neonatal HSV disease is acquired at 1 of 3 distinct times: intrauterine (in utero); peripartum (perinatal); and postpartum (postnatal)" [3] Among pregnant women in the United States, "greater than 60% are positive for HSV-1...Overall, 60–80% of neonatal herpes is associated with the primary or first-episode genital herpes acquired in close proximity to delivery."[4]
"maternal acquisition of new infection in late pregnancy, ... accounts for 60–80% of neonatal herpes"[5]
However, newborns have a limited immune system for the first 3 weeks of life, and even a kiss by a well-meaning friend or relative who bears a virus-shedding cold sore on the lips can cause infection in the newborn (albeit rarely).
Prevention and Treatment
Because HSV 2 is spread more commonly by sexual contact, it is easier to prevent than HSV 1. There is currently no vaccine available for either virus. Avoiding contact with people who have obvious sores helps reduce infection, and prophylaxis with commonly available antiviral drugs can help prevent transmission during the latent phase of the illness. Prophylaxis can also be given to reduce frequency and severity of attacks. Consistent and correct use of condoms reduces transmission.
References
- ↑ Sullivan M. Sams R 2nd. Jamieson B. Holt J. Clinical inquiries. What is the best test to detect herpes in skin lesions?. Journal of Family Practice. 55(4):346, 348, 2006 Apr.)
- ↑ Kirkland LG. New developments in the management of STDs. [Review] [10 refs] [Journal Article. Review] Nurse Practitioner. 31(12):12-21; quiz 22-3, 2006 Dec. UI: 17149130
- ↑ Kimberlin DW. Diagnosis of herpes simplex virus in the era of polymerase chain reaction. Pediatric Infectious Disease Journal. 25(9):841-2, 2006 Sep.
- ↑ Tita AT. Grobman WA. Rouse DJ. Antenatal herpes serologic screening: an appraisal of the evidence. [Review] [49 refs] [Journal Article. Review] Obstetrics & Gynecology. 108(5):1247-53, 2006 Nov. UI: 17077252
- ↑ Tita AT. Grobman WA. Rouse DJ. Antenatal herpes serologic screening: an appraisal of the evidence. [Review] [49 refs] [Journal Article. Review] Obstetrics & Gynecology. 108(5):1247-53, 2006 Nov. UI: 17077252
Goldman: Cecil Textbook of Medicine, 22nd ed., Copyright © 2004 W. B. Saunders Company
Cohen & Powderly: Infectious Diseases, 2nd ed., Copyright © 2004 Mosby, An Imprint of Elsevier
