Glycogen: Difference between revisions
imported>Pedro Silva No edit summary |
imported>David Tribe m (Protected "Glycogen" [move=sysop]) |
(No difference)
| |
Revision as of 06:06, 15 February 2007
Basic Histology, 11th ed, p49
Glycogen is a polysaccharide that is the principal storage form of glucose (Glc) in animal and human cells. Glycogen is found in the form of granules in the cytosol in many cell types. Hepatocytes (liver cells) have the highest concentration of it - up to 8% of the fresh weight in well fed state, or 100–120 g in an adult. In the muscles, glycogen is found in a much lower concentration (1% of the muscle mass), but the total amount exceeds that in liver. Small amounts of glycogen are found in the kidneys, and even smaller amounts in certain glial cells in the brain and white blood cells. Glycogen plays an important role in the glucose cycle.
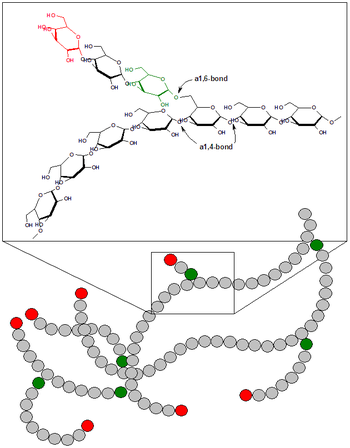
Structure and biochemistry
Glycogen is a highly branched polymer that is better described as a dendrimer of about 60,000 glucose residues and has a molecular weight between 106 and 107 daltons (4.8 million approx.). Most of Glc units are linked by α-1,4 glycosidic bonds, approximately 1 in 12 Glc residues also makes -1,6 glycosidic bond with a second Glc, which results in the creation of a branch. Glycogen does not possess a reducing end: the 'reducing end' glucose residue is not free but is covalently bound to a protein termed glycogenin as a β-linkage to a surface tyrosine residue. Glycogenin is a glycosyltransferase and occurs as a dimer in the core of glycogen. The glycogen granules contain both glycogen and the enzymes of glycogen synthesis (glycogenesis) and degradation (glycogenolysis). The enzymes are nested between the outer branches of the glycogen molecules and act on the non-reducing ends. Therefore, the many non-reducing end-branches of glycogen facilitate its rapid synthesis and catabolism.
Function and regulation of liver glycogen
As a carbohydrate meal is eaten and digested, blood glucose levels rise, and the pancreas secretes insulin. Glucose from the portal vein enters the liver cells (hepatocytes). Insulin acts on the hepatocytes to stimulate the action of several enzymes, including glycogen synthase. Glucose molecules are added to the chains of glycogen as long as both insulin and glucose remain plentiful. In this postprandial or "fed" state, the liver takes in more glucose from the blood than it releases.
After a meal has been digested and glucose levels begin to fall, insulin secretion is reduced, and glycogen synthesis stops. About four hours after a meal, glycogen begins to be broken down to be converted again to glucose. Glycogen phosphorylase is the primary enzyme of glycogen breakdown. For the next 8–12 hours, glucose derived from liver glycogen will be the primary source of blood glucose to be used by the rest of the body for fuel.
Glucagon is another hormone produced by the pancreas, which in many respects serves as a counter-signal to insulin. When the blood sugar begins to fall below normal, glucagon is secreted in increasing amounts. It stimulates glycogen breakdown into glucose even when insulin levels are abnormally high.
Glycogen in muscle and other cells
Muscle cell glycogen appears to function as an immediate reserve source of available glucose for muscle cells. Other cells that contain small amounts use it locally as well. Muscle cells lack the ability to pass glucose into the blood, so the glycogen they store internally is destined for internal use and is not shared with other cells, unlike liver cells.
Glycogen and marathon running
Due to the body's ability to hold no more than around 2,000 kcal of glycogen, marathon runners commonly experience a phenomenon referred to as "hitting the wall" around the 20 mile (32 km) point of a marathon. (Approximately 100 kcal are utilized per mile, depending on the size of the runner and the race course.) When experiencing glycogen debt, runners many times experience fatigue.
Disorders of glycogen metabolism
The most common disease in which glycogen metabolism becomes abnormal is diabetes, in which, because of abnormal amounts of insulin, liver glycogen can be abnormally accumulated or depleted. Restoration of normal glucose metabolism usually normalizes glycogen metabolism as well.
In hypoglycemia caused by excessive insulin, liver glycogen levels are high, but the high insulin level prevents the glycogenolysis necessary to maintain normal blood sugar levels. Glucagon is a common treatment for this type of hypoglycemia.
Various inborn errors of metabolism are caused by deficiencies of enzymes necessary for glycogen synthesis or breakdown. These are collectively referred to as glycogen storage diseases.
External links