Estrogen: Difference between revisions
imported>Robert Badgett |
mNo edit summary |
||
| Line 29: | Line 29: | ||
== External Links == | == External Links == | ||
{{CZMed}} | {{CZMed}}[[Category:Suggestion Bot Tag]] | ||
Latest revision as of 16:00, 13 August 2024
An estrogen is a type of steroid hormone with eighteen carbons. With increasing age and menopause, the levels of estrogens decrease in women, and estrogen replacement therapy has been used for decades to decrease the systoms associated with menopause. However, recent studies suggest that estrogen replacement therapy increases the risks of heart attacks and strokes, so its use is now declining. The steroids estrone and estradiol are both estrogens.
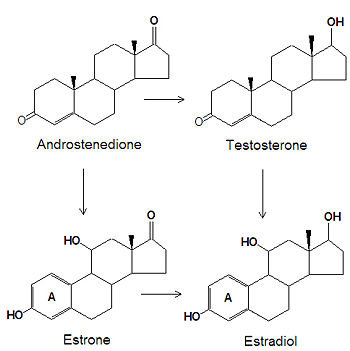
Biosynthesis
The estrogens are biosynthesized, by several chemical modifications of androgens. The C-3 ketone group is reduced to an alcohol, the C-19 methyl group is removed and the "A" ring (see steroid for numbering and nomenclature) becomes an aromatic ring.
Estrogen replacement therapy (ERT)
Cardiovascular disease
Originally thought to reduce vascular disease[1], the increase in cardiovascular mortality observed during the HERS[2] and Women's Health Initiative (WHI) [3][4] randomized controlled trials has led several practitioners to cease recommending hormone replacement therapy to most of their menopausal patients.[5]
There is conflicting evidence regarding increased risk of cardiovascular disease among women who start hormone replacement therapy soon after menopause. These patients may[6] or may not[7] be at increased risk of harms. Thus HRT may be an acceptable treatment of vasomotor symptoms in women less than 60 years old, have been menopausal for less than 10 years, are treated with statins, and have a lipid profile and a body weight that are satisfactory. This combination of factors is not rare.[8] In addition, women with risk of thrombotic disease should avoid HRT.[9]
The adverse outcomes seen in the WHI trial are not necessarily direct consequences of the treatment, but can result from an exacerbation by estrogen and progestogen of other abnormalities associated with menopause, aging or other factors. Seelig & al have explained how the grossly abnormal calcium:magnesium ratio seen in most of the women who participated to the trial (and most age-matched women in the USA, for instance) likely caused the adverse events; estrogen function depends on normal tissue magnesium concentrations and calcium:magnesium ratios.[10]
Venous thrombosis
A secondary analysis of the WHI reported increased venous thrombosis for participants of all ages with greater risk occurring in older women.[9]
Cognition
Estrogen does not improve cognitive function among postmenopausal women according to a systematic review of randomized controlled trials by the Cochrane Collaboration[11]
21-hydroxylase deficiency
References
- ↑ American College of Physicians. 1992 http://pubmed.gov/1443971
- ↑ Hulley S, Grady D, Bush T, et al (1998). "Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group". JAMA 280 (7): 605–13. PMID 9718051. [e]
- ↑ Rossouw JE, Anderson GL, Prentice RL, et al (2002). "Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial". JAMA 288 (3): 321–33. PMID 12117397. [e]
- ↑ Anderson GL, Limacher M, Assaf AR, et al (2004). "Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial". JAMA 291 (14): 1701–12. DOI:10.1001/jama.291.14.1701. PMID 15082697. Research Blogging.
- ↑ Austin PC, Mamdani MM, Tu K, Jaakkimainen L (2003). "Prescriptions for estrogen replacement therapy in Ontario before and after publication of the Women's Health Initiative Study". JAMA 289 (24): 3241–2. DOI:10.1001/jama.289.24.3241. PMID 12824204. Research Blogging.
- ↑ Prentice RL et al. Benefits and risks of postmenopausal hormone therapy when it is initiated soon after menopause. Am J Epidemiol. 2009 Jul 1;170(1):12-23. PMID 19468079
- ↑ Rossouw JE, Prentice RL, Manson JE, et al (2007). "Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause". JAMA 297 (13): 1465–77. DOI:10.1001/jama.297.13.1465. PMID 17405972. Research Blogging.
- ↑ Neves-E-Castro M (2003). "Menopause in crisis post-Women's Health Initiative? A view based on personal clinical experience". Hum. Reprod. 18 (12): 2512–8. PMID 14645165.
- ↑ 9.0 9.1 Cushman M, Kuller LH, Prentice R, et al (2004). "Estrogen plus progestin and risk of venous thrombosis". JAMA 292 (13): 1573–80. DOI:10.1001/jama.292.13.1573. PMID 15467059. Research Blogging.
- ↑ Seelig MS, Altura BM, Altura BT (2004). "Benefits and risks of sex hormone replacement in postmenopausal women". J Am Coll Nutr 23 (5): 482S–496S. PMID 15466949.
- ↑ Lethaby A, Hogervorst E, Richards M, Yesufu A, Yaffe K (2008). "Hormone replacement therapy for cognitive function in postmenopausal women". Cochrane Database Syst Rev (1): CD003122. DOI:10.1002/14651858.CD003122.pub2. PMID 18254016. Research Blogging.
External Links
The most up-to-date information about Estrogen and other drugs can be found at the following sites.
- Estrogen - FDA approved drug information (drug label) from DailyMed (U.S. National Library of Medicine).
- Estrogen - Drug information for consumers from MedlinePlus (U.S. National Library of Medicine).
- Estrogen - Detailed information from DrugBank.