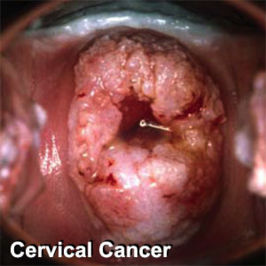
Cervical cancer: Difference between revisions
imported>Robert Badgett |
mNo edit summary |
||
| (2 intermediate revisions by one other user not shown) | |||
| Line 3: | Line 3: | ||
==Screening== | ==Screening== | ||
===Clinical practice guidelines=== | ===Clinical practice guidelines=== | ||
[[Clinical practice guideline]]s by the [[U.S. Preventive Services Task Force]] guide screening: | [[Clinical practice guideline]]s by the [[U.S. Preventive Services Task Force]] guide screening:<ref>{{cite web |url= http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm |title=Screening for Cervical Cancer |author=[U.S. Preventive Services Task Force |work=uspreventiveservicestaskforce.org |year=2012 [last update] |accessdate=March 15, 2012}}</ref> | ||
* "The USPSTF recommends screening for cervical cancer in women ages 21 to 65 years with cytology (Pap smear) every 3 years or, for women ages 30 to 65 years who want to lengthen the screening interval, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years. See the Clinical Considerations for discussion of cytology method, HPV testing, and screening interval." | * "The USPSTF recommends screening for cervical cancer in women ages 21 to 65 years with cytology (Pap smear) every 3 years or, for women ages 30 to 65 years who want to lengthen the screening interval, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years. See the Clinical Considerations for discussion of cytology method, HPV testing, and screening interval." | ||
* "The USPSTF recommends against screening for cervical cancer in women who have had a hysterectomy with removal of the cervix and who do not have a history of a high-grade precancerous lesion (i.e., cervical intraepithelial neoplasia [CIN] grade 2 or 3) or cervical cancer." | * "The USPSTF recommends against screening for cervical cancer in women who have had a hysterectomy with removal of the cervix and who do not have a history of a high-grade precancerous lesion (i.e., cervical intraepithelial neoplasia [CIN] grade 2 or 3) or cervical cancer." | ||
* "The USPSTF recommends against screening for cervical cancer with HPV testing, alone or in combination with cytology, in women younger than age 30 years." | * "The USPSTF recommends against screening for cervical cancer with HPV testing, alone or in combination with cytology, in women younger than age 30 years." | ||
| Line 58: | Line 56: | ||
* [[sensitivity (tests)|sensitivity]] 100%<ref name="pmid17942871"/> | * [[sensitivity (tests)|sensitivity]] 100%<ref name="pmid17942871"/> | ||
* [[specificity (tests)|specificity]] 93%<ref name="pmid17942871"/> | * [[specificity (tests)|specificity]] 93%<ref name="pmid17942871"/> | ||
===Specimen collection=== | |||
"The widely used Ayre's spatula is the least effective device for cervical sampling and should be superseded by extended-tip spatulas for primary screening and investigation of women before and after treatment for cervical intraepithelial neoplasia" according to a [[meta-analysis]]. <ref name="pmid10577637">{{cite journal| author=Martin-Hirsch P, Lilford R, Jarvis G, Kitchener HC| title=Efficacy of cervical-smear collection devices: a systematic review and meta-analysis. | journal=Lancet | year= 1999 | volume= 354 | issue= 9192 | pages= 1763-70 | pmid=10577637 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10577637 }} </ref> | |||
===Effectiveness of screening=== | ===Effectiveness of screening=== | ||
| Line 65: | Line 66: | ||
==References== | ==References== | ||
<references/> | <references/>[[Category:Suggestion Bot Tag]] | ||
Latest revision as of 16:00, 26 July 2024
Screening
Clinical practice guidelines
Clinical practice guidelines by the U.S. Preventive Services Task Force guide screening:[1]
- "The USPSTF recommends screening for cervical cancer in women ages 21 to 65 years with cytology (Pap smear) every 3 years or, for women ages 30 to 65 years who want to lengthen the screening interval, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years. See the Clinical Considerations for discussion of cytology method, HPV testing, and screening interval."
- "The USPSTF recommends against screening for cervical cancer in women who have had a hysterectomy with removal of the cervix and who do not have a history of a high-grade precancerous lesion (i.e., cervical intraepithelial neoplasia [CIN] grade 2 or 3) or cervical cancer."
- "The USPSTF recommends against screening for cervical cancer with HPV testing, alone or in combination with cytology, in women younger than age 30 years."
The American Cancer Society recommends similar screening.[2]
In additional, clinical practice guidelines address mass screening for cervical cancer by the American College of Obstetricians and Gynecology.[3]. A summary of these guidelines is:[4]
- "Cervical cancer screening should begin at age 21 regardless of age at onset of sexual activity."
- "Cervical cytology screening from age 21 to 29 is recommended every 2 years but should be more frequent in women who are HIV-positive, are immunosuppressed, were exposed in utero to diethylstilbestrol, or have been treated for cervical intraepithelial neoplasia (CIN) 2, 3 or cervical cancer."
- "Women age 30 who have three consecutive negative screens and who do not fit the above criteria for more-frequent screening may be tested every 3 years. Co-testing with cervical cytology and high-risk HPV typing is also appropriate; if both tests are negative, rescreening in 3 years is warranted."
- "Cervical cancer screening is unnecessary in women who have undergone hysterectomies for benign disease and who have no histories of CIN."
- "Discontinuation of screening after age 65 or 70 is reasonable in women with 3 negative consecutive tests and no cervical abnormalities during the previous decade."
- "Women with histories of CIN 2, 3 or cancer should undergo annual screening for 20 years after treatment."
- "HPV vaccination does not change these recommendations."
Accuracy of screening tests
Papanicolaou smear
A systematic review of available studies for detection of cervical intraepithelial neoplasia grade 2 or worse found the follow results.[5]
| ASCUS or worse | High grade or worse | |||
|---|---|---|---|---|
| sensitivity | specificity | sensitivity | specificity | |
| Conventional method | 88% | 71% | 55% | 97% |
| Liquid-based thin prep | 88% | 71% | 57% | 97% |
A more recent study of the conventional method for cervical intraepithelial neoplasia of grade 2 or 3 reported very similar results:[6]
- sensitivity 55%
- specificity 94%
Human papillomavirus testing
- sensitivity 95%[6]
- specificity 97%[6]
Combined testing
If either the Papanicolaou smear or Human papillomavirus testing are abnormal:
- sensitivity 100%[6]
- specificity 93%[6]
Specimen collection
"The widely used Ayre's spatula is the least effective device for cervical sampling and should be superseded by extended-tip spatulas for primary screening and investigation of women before and after treatment for cervical intraepithelial neoplasia" according to a meta-analysis. [7]
Effectiveness of screening
In a randomized controlled trial, the addition of Human papillomavirus testing to screening for cervical cancer "reduces the incidence of grade 2 or 3 cervical intraepithelial neoplasia or cancer detected by subsequent screening examinations."[8]
In another randomized controlled trial, the addition of Human papillomavirus testing to screening for cervical cancer led to earlier detection of CIN3+ lesions.[9]
References
- ↑ [U.S. Preventive Services Task Force (2012 [last update]). Screening for Cervical Cancer. uspreventiveservicestaskforce.org. Retrieved on March 15, 2012.
- ↑ Saslow, Debbie; Diane Solomon, Herschel W Lawson, Maureen Killackey, Shalini L Kulasingam, Joanna Cain, Francisco A. R Garcia, Ann T Moriarty, Alan G Waxman, David C Wilbur, Nicolas Wentzensen, Levi S Downs Jr, Mark Spitzer, Anna‐Barbara Moscicki, Eduardo L Franco, Mark H Stoler, Mark Schiffman, Philip E Castle, Evan R Myers. "American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer". CA: A Cancer Journal for Clinicians. DOI:10.3322/caac.21139. ISSN 1542-4863. Retrieved on 2012-03-15. Research Blogging.
- ↑ (2009) Cervical Cytology Screening. The American College of Obstetricians and Gynecology
- ↑ Davis AJ. (2009) Major Changes in ACOG Cervical Cytology Screening Recommendations. Journal Watch Women's Health
- ↑ 5.0 5.1 Arbyn M, Bergeron C, Klinkhamer P, Martin-Hirsch P, Siebers AG, Bulten J (2008). "Liquid Compared With Conventional Cervical Cytology: A Systematic Review and Meta-analysis". Obstet Gynecol 111 (1): 167–177. DOI:10.1097/01.AOG.0000296488.85807.b3. PMID 18165406. Research Blogging.
- ↑ 6.0 6.1 6.2 6.3 6.4 Mayrand MH, Duarte-Franco E, Rodrigues I, et al (2007). "Human papillomavirus DNA versus Papanicolaou screening tests for cervical cancer". N. Engl. J. Med. 357 (16): 1579–88. DOI:10.1056/NEJMoa071430. PMID 17942871. Research Blogging.
- ↑ Martin-Hirsch P, Lilford R, Jarvis G, Kitchener HC (1999). "Efficacy of cervical-smear collection devices: a systematic review and meta-analysis.". Lancet 354 (9192): 1763-70. PMID 10577637. [e]
- ↑ Naucler P, Ryd W, Törnberg S, et al (2007). "Human papillomavirus and Papanicolaou tests to screen for cervical cancer". N. Engl. J. Med. 357 (16): 1589–97. DOI:10.1056/NEJMoa073204. PMID 17942872. Research Blogging.
- ↑ Bulkmans NW, Berkhof J, Rozendaal L, et al (2007). "Human papillomavirus DNA testing for the detection of cervical intraepithelial neoplasia grade 3 and cancer: 5-year follow-up of a randomised controlled implementation trial". Lancet 370 (9601): 1764–72. DOI:10.1016/S0140-6736(07)61450-0. PMID 17919718. Research Blogging.